Quality of care and relationships as reported by children with cancer and their parents
Introduction
Cancer is a disease of aging; its occurrence in childhood is rare with a lifetime incidence of less than 0.5% (1). Despite this rarity, cancer remains the second most common cause of death after accidents and assault, and the leading cause of disease-related death in children (2). Cancer and its treatment cause considerable symptom burden on the patient, ranging from physical symptoms to psychological, social, and spiritual concerns (3). These concerns may increase the patient’s symptom burden, significantly impair quality of life, and limit possible curative treatments (3). Not only does cancer affect the patient, but also the whole family of the patient’s. Having a child diagnosed with a progressive life-threatening illness such as cancer has an emotional, physical, financial, and spiritual impact on the whole family. Parents develop emotional distress and depression, become physically exhausted, and suffer financial hardships due to treatment-related expenses and loss of income from repetitive work disruptions (4).
Palliative care (PC), according to the World Health Organization (5), is the approach that improves the quality of life of patients and families facing a life-limiting disease. This may be achieved through effective symptom management as well as spiritual and psychological support from diagnosis till end of life and bereavement. PC is defined as “the active, total care of the child’s body, mind and spirit, and also involves giving support to the family. It begins when illness is diagnosed, and continues regardless of whether or not a child receives treatment directed at the disease” (5). The aim of PC, according to Waldman & Wolfe (6), is to help the child live better taking into consideration the diagnosis limitations, the child’s goals, and the ways that the medical staff can use to help facilitate the achievement of these goals.
In Lebanon, the need for PC was first identified in 1995 at the WHO National Cancer Control Workshop (7). The importance of integrating PC in the plan of care of every child with cancer and developing hospice care for terminally ill children were emphasized in two case reports from the Children’s Cancer Centre of Lebanon (8). Lack of knowledge and absence of clear standards on PC among nurses working in Lebanese hospitals were found in a national study conducted by Abu-Saad Huijer et al. (9). In this study, only 20.2% of pediatric nurses and 3.7% of pediatricians received any form of education in PC, and pediatric nurses considered that the patient’s family should be involved in the treatment choice more than pediatricians. While 93% of pediatric nurses and 92.6% of pediatricians believed that the patient should be informed of the diagnosis, only 6.3% of these pediatric nurses and 23.5% of pediatricians actually informed patients of their diagnosis. A study by Saad et al. (10) evaluating the quality of care provided to children with cancer during their last months of life as perceived by bereaved parents showed that although the communication with the healthcare team and the quality of care delivered were mostly rated as “very good” to “excellent”, children suffered from fatigue, anorexia, depression, pain, and edema before they died. While 93.1% of parents reported having a discussion with the healthcare team about the bad news regarding the child’s health during the last month of life, only one third of parents reported their involvement in decision-making regarding resuscitation interventions and home-based care versus hospital-based care. Another qualitative study by Khoury et al. (11) described the parents’ experience having a child with cancer as a “continuous battle” that negatively affected the family’s way of living, parental relationship, and sibling rivalry. A recent study, conducted by Abu-Saad Huijer et al. (12) on the quality of PC among children with cancer aged 7 to 18 years, showed that children had a satisfactory quality of life. Lack of appetite, pain, and nausea were the symptoms most commonly reported by children (7 to 12 years), while lack of energy, irritability, and pain was most commonly experienced by adolescents (13 to 18 years). The symptoms most frequently treated were pain and nausea. The results of the same study, taking the parents’ perspectives into consideration, showed that children faced health-related quality of life problems in terms of nausea, worry, and treatment anxiety. Parents reported irritability, nervousness, lack of energy, lack of appetite, pain, and feeling sad as the most prevalent symptoms, while nausea, vomiting, cough, and pain were reported as the most treated symptoms (12,13).
This article is based on the studies conducted by Abu-Saad Huijer et al. (12,13) that focus primarily on exploring the experience of children currently living with cancer and receiving PC as well as that of their parents. The article focuses on evaluating the quality of PC in terms of quality of medical care received, effect of cancer on patients’ relationships, degree of patients’ spirituality/religiousness, and degree of parents’ financial hardships during their child’s diagnosis with cancer.
The study objectives are as follows: (I) to assess the quality of PC in terms of access to care, patient-clinician relationship, and clinician communication, as viewed by patients and parents; (II) to assess the degree of spirituality/religiousness of patients and their sense of purpose after getting diagnosed with cancer, as reported by both patients and parents; (III) to explore the effect of cancer on the patients’ relationships including friendships and social connections as viewed by patients and parents, and acceptance of death as well as preparing others for the idea of losing the child as viewed by parents only, and (IV) to assess the degree of financial hardship during the child’s illness, as reported by parents.
Materials and methods
Research design
The study was conducted using a cross-sectional, descriptive, quantitative design that targeted patients living with cancer and their parents at a tertiary pediatric cancer center in Lebanon. Through personal interviews with the children and the parents, the quality of medical care received and the effect of illness on patients’ spirituality/religiousness and relationships were evaluated (as reported by patients and parents). The parent’s financial hardships during their child’s illness were explored as well (as reported by parents only). The study was approved by the American University of Beirut Institutional Review Board.
Settings and sample
A tertiary pediatric cancer center was chosen as the primary data collection site for this study. This center is considered a referral center for pediatric oncology in the region and receives Lebanese as well as non-Lebanese patients from different Arab countries.
Between 2010 and 2011, a non-probability convenience sample of 85 children and adolescents between the ages of 7 to 18 years was enrolled in the study. The inclusion criteria included Lebanese and non-Lebanese patients diagnosed with cancer for more than one month, know about their disease, are receiving cancer treatment, have assented or consented to participate in the study, and were accompanied by a parent or a significant other who would consent their participation. The parents or significant others directly involved in the care of these children were included in the study.
The research assistant visited the inpatient and outpatient clinics on a daily basis and identified eligible patients with the assistance of the nurse managers of the two units.
Data collection procedures
After securing the informed consents of parents and assents of children and adolescents, the research assistant conducted face-to-face interviews with parents, adolescents, and children separately. The interviews with patients took place either in the patients’ hospital rooms for admitted patients or in the outpatient private conference room for patients receiving their treatment in the outpatient unit. The interviews with parents took place in the private conference rooms of the two units. The interviewer read the questions, reread them if the participant did not understand, explained the rating scales, and documented the answers of the interviewees only.
Translation, cultural validity, and pilot study
The original English version of the questionnaire was translated into Lebanese Arabic, following the back-translation procedure. The questionnaire was initially translated into Arabic by one of the researchers. The translated version was sent to two experts in the Arabic language for evaluation where minor grammatical changes were noted. Another independent translator, with no knowledge of the English version, carried out the backward-translation. The translated version was compared with the original English version for consistency and accuracy. This procedure is the preferred method to be used when translating research items since it preserves the equivalent meaning of items in both languages (14). In order to culturally validate the research instrument, a team of four experts, two in PC and two in research design and instrument development, rated the Arabic version of the questionnaire. The recommendations were to change the negatively worded items from the Needs at End of Life Screening Tool (NEST) questionnaire to positively worded ones.
The questionnaire in its Arabic version was pilot tested on four oncology patients from the two age groups. The participants reported no problems or difficulties and no further changes were applied.
Research instrument
NEST questionnaire was used in this study. The different domains of this tool, which was initially created to evaluate end-of-life care as experienced by adult patients, have shown content and construct validity as well as internal reliability with Cronbach’s α coefficients ranging from 0.64 to 0.86 (15). This tool is applicable to patients of different age groups, with a wide range of diagnoses, having different social circumstances, and receiving treatment in different care settings (15,16). For the parents’ interviews, 23 items were selected from the initial questionnaire targeting different domains: financial burden (3 items), quality of medical care (10 items), spirituality/religiousness (6 items), and relationships (4 items). As for the children’s and adolescents’ questionnaires, 12 items were selected targeting quality of medical care (5 items), spirituality/religiousness (4 items), and relationships (3 items). The response format of the NEST followed a 1 to 10 scale, where higher scores on the domains related to quality of medical care, spirituality/religiousness, and relationships indicated better quality of the measured concept; however, higher scores on the financial burden domain indicated higher financial difficulties. Some negatively worded items on the NEST questionnaire were changed into positively worded ones. In the parents’ questionnaire the answers of three items pertaining to the quality of medical care were reversed. In the children and adolescents’ questionnaires the answers of five items pertaining to the quality of medical care and the answer of one item pertaining to spirituality were reversed as well.
The questionnaire included a section on the demographic and clinical characteristics of patients, including questions about the patient’s age, gender, cancer diagnosis and stage, type of treatment received, educational status, and days skipped from school. The demographic characteristics of parents included questions about the relation to the child, educational level, and employment.
Statistical analysis
The demographic characteristics of parents and patients and the clinical characteristics of patients were analyzed using frequencies (N) and percentages (%). Independent sample t-tests were used to test the differences in mean scores of the NEST subscales in terms of patient’s age and gender. Independent sample t-tests were also used to test the differences in mean scores of two separate questions about healthcare providers’ goodness in providing care and their sensitivity to patients’ needs in terms of patient’s age and gender. Data management and analyses were done using SPSS software version 20.
Results
Sample characteristics
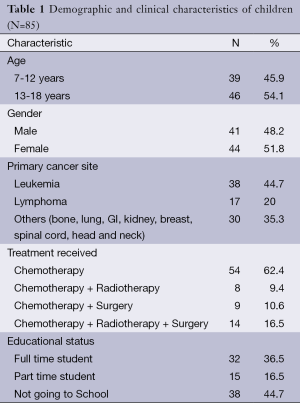
A sample of 85 pediatric oncology patients participated in the study over a one-year period. Approximately 14 patients (14.1%) refused to participate as they reported feeling tired, sleepy, or preferred to play or watch television, resulting in a response rate of 85.9%. The patients were almost equally distributed in terms of age: children aged 7 to 12 years amounted to 45.9%, and adolescents aged 13 to 18 years amounted to 54.1%. As for gender, 48.2% were male and 51.8% were female. Most of the patients (82.4%) were receiving their treatments at the outpatient unit. Almost half (44.7%) had leukemia and one fifth (20%) had lymphoma. More than half of the patients (62.4%) were receiving chemotherapeutic regimens only. Almost half of the patients (44.7%) reported not going to school, while among those going to school, a mean of 2.54 months was reported as the time skipped from school during the past six months (Table 1).
Full table
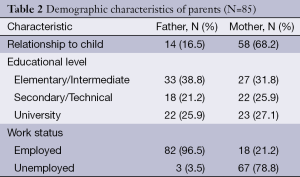
A total of 85 parents were enrolled in the study. Out of the 88 parents approached, only three refused to participate because they were preoccupied with their children’s admission papers, yielding a response rate of 96.6%. Approximately two thirds of parents (68.2%) were mothers and 16.5% were fathers. Around one third of mothers (31.8%) and 38.8% of fathers had up to elementary/intermediate educational level. Most of the mothers (78.8%) reported that they were unemployed, while the majority of fathers (96.5%) were employed (Table 2).
Full table
Needs at End of Life Screening Tool (NEST)
Children and adolescents
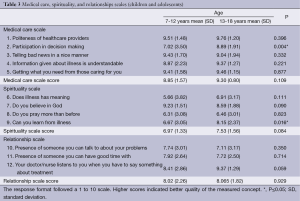
On a scale of 1 to 10, children had a mean score (M) of 8.85 on the medical care scale and a standard deviation (SD) of 1.57, indicating a very good quality of medical care. The highest scores were almost equally given for politeness of healthcare providers (M =9.51, SD =1.48), being nice in telling bad news (M =9.43, SD =1.70), and giving patients exactly what they need (M =9.4, SD =1.58). The lowest score was for participation in decision-making (M =7.02, SD =3.50).
Adolescents reported excellent quality of medical care (M =9.30, SD =0.80). The highest score was given for politeness of healthcare providers (M =9.76, SD =1.20), while the lowest score was given for participation in decision-making (M =8.89, SD =1.91). When compared by age, one significant difference was found with respect to participation in decision-making (P=0.004), where adolescents reported more participation in decision making than children.
Regarding spirituality and religiousness, children reported good spirituality (M =6.97, SD =1.33) with the highest score given for the belief in God (M =9.23, SD =1.51) and the lowest score for meaning of illness (M =5.66, SD =3.82). Adolescents reported better spirituality (M =7.53, SD =1.56). The highest score being for the belief in God (M =8.59, SD =1.88) and lowest score for praying more after getting diagnosed with illness (M =6.46, SD =3.01).
When compared for age, adolescents showed more readiness to learn from illness than children (P=0.016).
With regard to the relationship scale, children considered that doctors/nurses are good listeners (M =8.02, SD =2.26), but expressed some need for the presence of someone to talk to about problems (M =7.74, SD =3.01). Almost same results were seen in adolescents as well (Table 3).
Full table
Parents
On a scale of 1 to 10, parents gave a mean score of 5.35 (SD =2.60) on the financial burden scale, indicating a moderate financial hardship during the child’s illness. When compared for age, parents of adolescents reported more difficulties in getting insurance to cover illness expenses than parents of children (P=0.036).
When asked to rate the quality of medical care, parents gave high scores indicating a high quality of care (M =8.83, SD =0.92). The parents of children and adolescents were mostly satisfied with the respect of nurses and doctors toward the child (M =9.85, SD =0.52), and least satisfied with securing a hospital bed (M =6.87, SD =3.38). When compared for age, parents of adolescents showed that the medical care fits with their goals and their child’s goals more than the parents of children (P=0.045). When compared for gender, parents of male patients reported more satisfaction with respect to coordination of doctors with other healthcare providers (P=0.034) than parents of female patients.
With respect to spirituality, parents reported a good spirituality level among their children (M =7.86, SD =1.62). The highest scores were given for the degree of the child’s spirituality (M =9.35, SD =1.34), while the lowest scores for the sense and meaning of illness to the child (M =6.13, SD =3.97). When compared for age, parents reported that children’s sense of purpose seems to be more affected by religious belief than adolescents (P=0.029).
When asked about relationships, parents gave a mean score of 7.53 (1.25) considering healthcare providers as excellent listeners to parents and patients 9.42 (1.15); however, they reported not preparing others for the possibility of child’s death 3.21 (3.29). When compared for age, parents considered that children spend a good time with people more than adolescents (P=0.037) (Table 4).

Full table
Discussion
The most prevalent cancer type among children was leukemia followed by lymphoma. This is congruent with the distribution of cancer among children in Lebanon where leukemias and lymphomas are the most prevalent childhood cancers (17). Mothers who accompanied their children to receive their treatments contributed to 68.2% of the sample. Other studies interviewing parents of children with cancer have also shown that mothers constitute the majority of respondents (10,11,18-20). 85.9% of fathers and 84.7% of mothers had elementary or intermediate education and more. These results are consistent with the adult literacy rate in Lebanon, which was approximately 90% in 2007 (21).
All respondents reported high quality of medical care. A Lebanese study by Saad et al. (10) showed that 93.1% of bereaved parents rated the overall quality of care as “very good” and “excellent”. Another study by Wolfe et al. (22) found 81% of bereaved parents to be satisfied with the overall quality of care rating it as very good or excellent. Patients in this study were mostly satisfied with the politeness of healthcare providers, getting from them what they need, and their nice way in telling bad news. Parents were mainly satisfied with the respect of nurses and doctors toward the child, the presence of a good follow-up system, and the coordination between healthcare professionals. A study by Hsiao et al. (19) has also shown that patients as well as parents appreciated doctors who took time with their patients, developed friendships with them, and demonstrated respect. Another study by Gilmer et al. (18) has shown that bereaved parents reported satisfaction with the availability of healthcare providers, the adequacy of information received about the child’s diagnosis, and symptom management. Contrary to the results of this study, parents and children in other studies have expressed dissatisfaction with the insensitive way some doctors used to break bad news (19,23). At the tertiary pediatric cancer center in Lebanon, parents and children are satisfied with the way physicians break bad news. This could be explained by the fact that attending physicians who break bad news are certified by the American Board of Pediatrics and well trained in PC, or parents and children think that their approach is best to break bad news.
Parents reported least satisfaction in securing a hospital bed followed by participating in decision-making. Securing a hospital bed at this cancer center is a major problem since the number of inpatient beds is limited and some patients have their treatments delayed until the availability of an empty bed.
The parents’ low participation in decision making has been mentioned previously by Saad et al. (10), where only one third of bereaved parents reported discussing resuscitation interventions and home care options with physicians. Patients also reported least satisfaction with participation in decision-making, though adolescents expressed more participation than children. Studies have also shown that children and parents desire more active involvement in decision-making (18-20,23). Adolescents’ involvement in decision-making as well as their readiness to learn from illness more than children is due to their cognitive development and their awareness of the overall experience that they are passing through, in addition to their cognitive ability to better understand the given information and take wiser decisions. This finding is in line with Hinds et al. (20) who found that patients between 10 and 20 years of age were able to fully participate in end-of-life decisions. Parents of adolescents reported better fitness of medical care with their goals more than parents of children and this could be explained by the fact that adolescents are allowed to participate in decision making more than children.
An important remark about the quality of medical care is the high satisfaction rates seen among patients and their parents despite lack of optimal symptom management. The study by Abu-Saad Huijer et al. (12) has shown that despite treating pain, nausea, and other symptoms, success rates in children were between 77.8% and 80%, while in adolescents this ranged between 57.1% and 66.7%. Parents also reported lack of optimal symptom management with success rates for treating nausea, vomiting, and pain ranging between 66.7% and 73.7% (13). Bereaved parents reported the same discrepancy between high satisfaction rates and low symptom management (10). Waldman & Wolfe (24) discussed this issue further and considered that parents and children accept significant symptom burden thinking that this is the best that could be done. In our view, cultural differences could explain this discrepancy in Lebanon; there is a strong possibility that patients and parents did not expect complete symptom control simply because they did not know it was possible or that pain is an expectation of all patients and parents when ill. The results of the study showed good levels of spirituality/religiousness among children, adolescents, and parents accompanied by strong faith and belief in God. In Lebanon, the issue of spirituality is strongly tied to religion; religious belief is of great importance since people of different religious sects live together and shares their belief in God. Spiritual and religious needs of children and parents in Lebanon are usually met by their religious leaders who provide support in the hospital and home settings when families are in need. The issue of spirituality/religiousness has also emerged with Lebanese adult oncology patients and their caregivers (25,26).
Patients and parents considered that healthcare providers were very good listeners when they had to say something about their treatment. The results of this study are in line with the results by Saad et al. (10) where 86.2% of bereaved parents rated the communication with healthcare providers as “very good” or “excellent”.
Parents in this study reported not preparing those around them for the possibility of their child’s death. This could have several explanations. First, parents reported strong faith in God and His ability to cure their children, which could leave them not accepting the idea of death and never losing hope in the possibility of a cure. Second, most of the interviewed parents and patients were chosen from the outpatient unit where patients usually come for a routine blood test or to receive chemotherapy, and the possibility of death may not be considered most of the time. Third, it could be that healthcare providers are reluctant in preparing either the family or the child for the possibility of death. This has been shown in the study by Saad et al. (10), where 31% of bereaved parents reported being “not at all” prepared for any emergencies in their child’s health and most of them had discussions about bad news only during the last month of the child’s life. Gilmer et al. (18) reported almost the same results where only 67% of bereaved parents said they were told that their child was dying. Bereaved parents in more than one study have expressed their desire to be prepared for the bad news and preferred if bad news had been delivered in a direct and honest manner while still allowing for hope (23,27). This lack of communication skills between patients, parents, and healthcare providers has not been only reported by parents and patients, but also by healthcare providers. Contro et al. (27) have shown that staff members in all occupations feel inexperienced communicating with patients and parents especially about issues related to end-of-life care. Pediatric healthcare providers in Lebanon have also shared similar concerns (9).
Parents of children in this study reported that their kids spend more time with people than adolescents. The cancer center has a psychotherapist, social worker, play therapist, teachers, and a number of volunteers who could be spending a great deal of time with children than with adolescents. Health care providers as a result, need to be more attentive to the special needs of adolescents during this period similar to the attention they give to children.
Knowing that the cancer center covers all the expenses of the child’s treatment, the results of the study have shown that parents suffer from a moderate financial hardship during their child’s illness. These financial hardships are mainly related to decreased or loss of employment, support in taking care of siblings at home, and lack of insurance to cover home care. Steele & Davies (4) also reported financial hardship expressed by parents who have a child with progressive life-threatening disease, which is mainly due to skipping days at work and to the expenses resulting from their child’s illness. Parents mainly reported significant difficulties in getting insurance plans to cover their child’s treatment due to some restrictions put by Lebanese insurance companies to cover certain cases and treatments. Parents of adolescents reported more difficulties than parents of children in getting insurance coverage to cover their children’s treatments. This could be due to the ignorance of parents about the importance of getting early insurance plans for their children before they are diagnosed. Financial hardship resulting from a child diagnosed with cancer has also been reported by Khoury et al. (11). The same concept of added burden has also been reported by caregivers of adult oncology patients (25,28).
Limitations
Selection bias is an important limitation in this study since the majority of patients and parents were recruited from an outpatient unit. Another limitation is the generalizability of the results. These results are taken from one center in Lebanon that has a limited number of pediatric oncology patients, uses advanced chemotherapeutic protocols, and has pediatric PC services. The results from this study therefore could not be generalized to the overall experience of having a child diagnosed with cancer in Lebanon. The cross-sectional design of this study is another limitation that does not provide a comprehensive picture of the overall experience with childhood cancer.
Recommendations
Based on the results of this study, improvement of PC services at the tertiary pediatric cancer center in Lebanon is highly recommended. A PC team that adequately addresses patients’ concerns and provides education to healthcare providers directly involved in the care of children with cancer is of utmost importance. Education shall focus on pain and symptom management as well as emotional and psychological support. It will also focus on communication with patients and parents, emphasizing the importance of patients’ and parents’ participation in decision making and conveying bad news. This study has shown that more social attention is given to children than adolescents: an issue that should be further addressed with the psychotherapist and the volunteers who provide a great deal of emotional and psychological support to parents and patients.
Acknowledgements
Dr. Huda Abu-Saad Huijer, Dr. Hala Darwish, and Ms. Rania Mosleh are kindly acknowledged for their authorship and significant contributions towards producing this study.
Disclosure: The authors of this study are all affiliated with the American University of Beirut, Lebanon and the American University of Beirut Medical Center. The authors confirm that no conflict of interest, financial or otherwise, exists, and that the content of this manuscript has not been published elsewhere.
References
- Finlay J, Carroll W. Cancer in Children and Adolescents. Sudbury: Jones and Bartlett Publishers, 2010.
- Friebert S. NHPCO Facts and Figures: Pediatric Palliative and Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization, 2009.
- Ferrell B, Paice J, Koczywas M. New standards and implications for improving the quality of supportive oncology practice. J Clin Oncol 2008;26:3824-31. [PubMed]
- Steele R, Davies B. Impact on parents when a child has a progressive, life-threatening illness. Int J Palliat Nurs 2006;12:576-85. [PubMed]
- World Health Organization. Palliative care [Internet]. 2014. Available online: http://www.who.int/cancer/palliative/en/
- Waldman E, Wolfe J. Palliative care for children with cancer. Nat Rev Clin Oncol 2013;10:100-7. [PubMed]
- Daher M, Estephan E, Abu-Saad Huijer H, et al. Implementation of palliative care in Lebanon: past, present, and future. J Med Liban 2008;56:70-6. [PubMed]
- Abboud MR, Azzi M, Muwakkit S. Pediatric Palliative Care at the Children’s Cancer Center of Lebanon: 2 Case Reports. Med Princ Pract 2007;16:50-2.
- Abu-Saad Huijer H, Abboud S, Dimassi H. Practices in pediatric PC in Lebanon. Eur J Palliat Care 2008;15:190-2.
- Saad R, Huijer HA, Noureddine S, et al. Bereaved parental evaluation of the quality of a palliative care program in Lebanon. Pediatr Blood Cancer 2011;57:310-6. [PubMed]
- Khoury MN, Huijer HA, Doumit MA. Lebanese parents' experiences with a child with cancer. Eur J Oncol Nurs 2013;17:16-21. [PubMed]
- Abu-Saad Huijer H, Sagherian K, Tamim H, et al. Quality of palliative care in children with cancer in Lebanon. J Med Liban 2013;61:228-36. [PubMed]
- Abu-Saad Huijer H, Sagherian K, Tamim H. Quality of life and symptom prevalence in children with cancer in Lebanon: the perspective of parents. Ann Palliat Med 2013;2:59-70.
- Frank-Stromborg M, Olsen SJ. eds. Instruments for clinical health-care research. Third edition. Boston: Jones and Bartlett Publishers, 2004.
- Emanuel LL, Alpert HR, Baldwin DC, et al. What terminally ill patients care about: toward a validated construct of patients' perspectives. J Palliat Med 2000;3:419-31. [PubMed]
- Emanuel LL, Alpert HR, Emanuel EE. Concise screening questions for clinical assessments of terminal care: the needs near the end-of-life care screening tool. J Palliat Med 2001;4:465-74. [PubMed]
- Noun P, Djambas-Khayat C. Current status of pediatric hematology/oncology and palliative care in Lebanon: a physician's perspective. J Pediatr Hematol Oncol 2012;34 Suppl 1:S26-7. [PubMed]
- Gilmer MJ, Foster TL, Bell CJ, et al. Parental perceptions of care of children at end of life. Am J Hosp Palliat Care 2013;30:53-8. [PubMed]
- Hsiao JL, Evan EE, Zeltzer LK. Parent and child perspectives on physician communication in pediatric palliative care. Palliat Support Care 2007;5:355-65. [PubMed]
- Hinds PS, Drew D, Oakes LL, et al. End-of-life care preferences of pediatric patients with cancer. J Clin Oncol 2005;23:9146-54. [PubMed]
- Lebanese Republic Ministry of Social Affairs. The National Survey of Household Living Conditions: A report of household living conditions 2007 [Internet]. 2008. Available online: http://www.socialaffairs.gov.lb
- Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med 2000;342:326-33. [PubMed]
- Contro N, Larson J, Scofield S, et al. Family perspectives on the quality of pediatric palliative care. Arch Pediatr Adolesc Med 2002;156:14-9. [PubMed]
- Waldman E, Wolfe J. High symptom burden in children with cancer and high parental satisfaction: why the disconnect? Ann Palliat Med 2013;2:54-55.
- Doumit MA, Huijer HA, Kelley JH, et al. The lived experience of Lebanese family caregivers of cancer patients. Cancer Nurs 2008;31:E36-42. [PubMed]
- Doumit MA, Abu-Saad Huijer H, Kelley JH. The lived experience of Lebanese oncology patients receiving palliative care. Eur J Oncol Nurs 2007;11:309-19. [PubMed]
- Contro NA, Larson J, Scofield S, et al. Hospital staff and family perspectives regarding quality of pediatric palliative care. Pediatrics 2004;114:1248-52. [PubMed]
- Schubart JR, Kinzie MB, Farace E. Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro Oncol 2008;10:61-72. [PubMed]


