Dyke-Davidoff-Masson syndrome: imaging features with illustration of two cases
Introduction
Dyke-Davidoff-Masson syndrome is a rare entity characterized by hemi cerebral atrophy/hypoplasia secondary to brain insult in fetal or early childhood period along with ipsilateral compensatory osseous hypertrophy and contralateral hemiparesis (1). We present two cases of this uncommon condition and discuss its imaging features, differential diagnosis, treatment options and prognosis.
Case report
Case 1
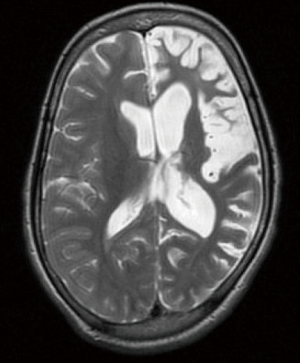
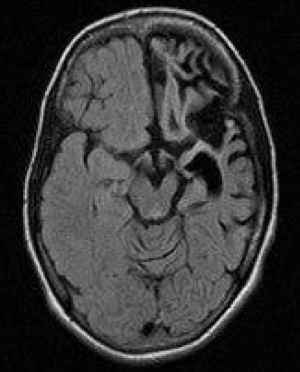
An 8-year-old male child presented with complaints of focal seizures, characterized by brief episodic movements of right side of body after which child regains consciousness. This started approximately at 1 year of age. The frequency of convulsions increased gradually and more so in the last four months. There was history of speech and language delay as well. His birth history and family history was unremarkable. On examination, patient had spastic hemiparesis on the right side. Treatment history revealed consulting local medical practitioner and patient was on carbamazepine. However, patient had stopped responding recently. Magnetic resonance imaging (MRI) of brain was advised which showed hemiatrophy of left cerebral hemisphere with ipsilateral dilated lateral ventricle and thickening of diploic space (Figures 1,2). Features were suggestive of Dyke-Davidoff-Masson syndrome. Other antiepileptic drugs were added in his medication and he almost became seizure free. He was advised speech therapy too and was kept on regular follow-ups.
Case 2
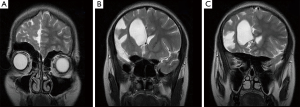
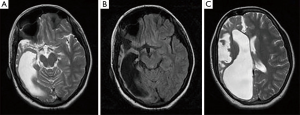
An 18-year-old female patient with history of seizures and left sided hemidystonia since last 12 years, presented to neurology outpatient department. General physical examination showed facial asymmetry and brisk left biceps and triceps reflexes and extensor plantar response on the left. MRI of brain showed hemicerebral atrophy on the right side with enlarged ipsilateral frontal and sphenoid sinuses, widened calvarium and elevated sphenoid and petrous ridge (Figures 3,4). Diagnosis of Dyke-Davidoff-Masson syndrome was made. Her treatment regime consisted of combination of anticonvulsant drugs along with physiotherapy and was kept on follow up.
Discussion
Dyke-Davidoff-Masson syndrome refers to variable degrees of hypoplasia or atrophy of one cerebral hemisphere with compensatory changes of the calvarium. The etiopathogenesis could be either vascular insult during intrauterine life resulting in hypoplasia of a cerebral hemisphere or acquired causes like trauma, infection, vascular abnormalities and intracranial hemorrhage in the perinatal period or shortly thereafter causing hemi cerebral atrophy. Cerebral atrophy in turn results due to reduction in the formation of brain derived neurotrophic factors by these causes (2,3).
The syndrome was first described by Dyke, Davidoff and Masson in 1933 on plain skull radiographs and pneumo-encephalograms in a series of nine patients. The clinical features depend on extent of brain injury and include hemiparesis or hemiplegia, seizures, mental retardation or learning disability, speech or language disorders and facial asymmetry. Rarely patients can also present with sensory symptoms and psychiatric disorders like schizophrenia. Nevertheless, seizures may appear months to years after the onset of hemiparesis and mental retardation is not seen in all cases (3-5).
The diagnosis is based on the typical radiological features on computed tomography (CT) and MRI scans which include cerebral hemiatrophy with dilated ipsilateral lateral ventricle. Also there is thickening of calvarium with enlargement of frontal, ethmoid and sphenoid sinuses and elevation of greater wing of sphenoid and petrous ridge. The osseous abnormalities can also be depicted on plain skull films (3).
The differential diagnoses are chronic Rasmussen encephalitis (chronic, progressive inflammation of brain of uncertain etiology) and sturge weber syndrome. However, Rasmussen encephalitis doesn’t show calvarial changes and sturge-weber syndrome additionally shows enhancing pial angiomas and cortical calcifications (3,6).
Management consists of control of seizures with appropriate anticonvulsants, as most patients with this disorder present with refractory seizures. Additionally, domiciliary physiotherapy, occupational and speech therapy have a crucial role. Hemispherectomy is indicated in patients with hemiplegia and intractable disabling seizures and is successful in 85% of the cases. Prognosis is poor in cases of prolonged or recurrent seizures and if hemiparesis occurs before two years of age. Hence, it is indeed very important for neurologists, paediatricians and radiologists to be familiar with this condition for its early diagnosis and treatment (3-6).
Disclosure: The authors declare no conflict of interest.
References
- Park KI, Chung JM, Kim JY. Dyke-davidoff-masson syndrome: cases of two brothers and literature review. J Epilepsy Res 2014;4:24-7. [PubMed]
- Lee JH, Lee ZI, Kim HK, et al. A case of Dyke-Davidoff-Masson syndrome in Korea. Korean J Pediatr 2006;49:208-11.
- Sharma S, Goyal D, Negi A, Sood RG, Jhobta A, Surya M. Dyke-davidoff masson syndrome. Indian J Radiol Imaging 2006;16:165-6.
- Singh P, Saggar K, Ahluwalia A. Dyke-Davidoff-Masson syndrome: Classical imaging findings. J Pediatr Neurosci 2010;5:124-5. [PubMed]
- Behera MR, Patnaik S, Mohanty AK. Dyke-Davidoff-Masson syndrome. J Neurosci Rural Pract 2012;3:411-3. [PubMed]
- Narain NP, Kumar R, Narain B. Dyke-Davidoff-Masson syndrome. Indian Pediatr 2008;45:927-8. [PubMed]