Glow in the dark
Image of the month
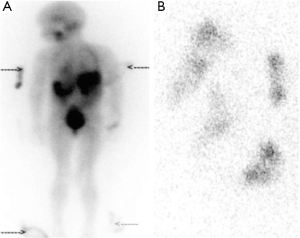
A 4-year-old girl with stage 4 neuroblastoma had a single-photon emission computer tomography (SPECT) scan three days after a therapeutic administration of radioactive 131I-meta iodobenzylguanidine (131I-mIBG). Figure 1A illustrates four radioactive areas (see arrows) outside her body contours in addition to the radioactive uptake in the metastases. It transpired that the child had been sucking at the four corners of her ‘comfort blanket’ throughout her treatment, which had also been used to cover her during the scan, resulting in radioactive contamination of the corners of the blanket. The blanket was scanned separately, confirming the nature of external abnormalities (Figure 1B).
Molecular radiotherapy with 131I-mIBG for neuroblastoma has been in clinical use for nearly 30 years. In this time, its role has changed from being an exclusively palliative treatment to one where the intent of treatment is often curative (1). Uptake of 131I-mIBG has been reported by Nakajo et al. in the salivary glands of patients undergoing scintigraphy for the location of suspected pheochromocytomas. This uptake of radioactivity was not due to free 131I derived from the 131I-mIBG but rather to uptake of 131I-mIBG by sympathetic neuronal elements in the salivary glands (2).
This illustrative case emphasizes that patient’s secretions remain radioactive for some time following treatment and highlights the importance of careful handling of radioactive secretions.
Disclosure: The authors declare no conflict of interest.
References
- Gaze MN, Gains JE, Walker C, Bomanji JB. Optimization of molecular radiotherapy with [131I]-meta Iodobenzylguanidine for high-risk neuroblastoma. Q J Nucl Med Mol Imaging 2013;57:66-78. [PubMed]
- Nakajo M, Shapiro B, Sisson JC, Swanson DP, Beierwaltes WH. Salivary gland accumulation of meta-[131I]iodobenzylguanidine. J Nucl Med 1984;25:2-6. [PubMed]


