The angle of pancreaticobiliary junction correlates with acute pancreatitis: a magnetic resonance cholangiopancreatography study
Introduction
Acute pancreatitis is a common and serious disease that often arises suddenly and has a high mortality rate (1-3). Hospital mortality increases from 1.6% in the youngest (0-14 years) to 11.4% in the oldest (≥85 years) individuals (2). The causes of pancreatitis include excessive alcohol consumption, biliary stones, traumas, autoimmunity, pancreatic tumors, genetic factors and several morphological anomalies, such as pancreaticobiliary malfunction, anatomical variants and pancreas divisum (1,4,5). The pathogenesis of acute pancreatitis involves the destruction of the self-defense system of the pancreas and activation of self-digestion with proenzymes. The defense mechanism of the pancreas is based on its anatomical and morphological structure.
The anatomic factors and mechanisms leading to acute pancreatitis remain to be further investigated (4). Some scholars (6-9) investigated the relationship between the anatomy of the pancreaticobiliary junction and acute pancreatitis, including the type of pancreaticobiliary ductal system, the shape and size of the pancreatic duct, the pancreaticobiliary common channel, the pancreaticobiliary intraductal pressure and the anatomy of the ampulla. They believed that anatomical variants might be a relevant factor with respect to the onset of acute pancreatitis, such as a meandering main pancreatic duct and the terminal shape of the accessory pancreatic duct (6,10). In addition, the main pancreatic duct width may be related to pancreatic diseases (7). However, this hypothesis has not confirmed by anatomical-pathological or clinical observations, and controversies exist among the research results (4,8,9,11).
To the best of our knowledge, no previous study has investigated the correlation between the angle of the pancreaticobiliary junction (APJ) and the prevalence of acute pancreatitis. Magnetic resonance cholangiopancreatography (MRCP), which is widely used in the clinic, is a noninvasive and multidirectional imaging technology that can also clearly display the anatomical structure of the pancreaticobiliary duct system (12). Pancreatic anatomical variants provided a direction for our research.
Materials and methods
Patient population
This study was approved by our institutional review board. Patient informed consent was signed. Between February 2014 to October 2014 at our institution, MRI examinations were performed in 98 patients in whom acute pancreatitis was excluded and in whom acute pancreatitis was clinically suspected.
To study the normal anatomy of the pancreaticobiliary junction, the normal subjects (group A) were selected as follows: firstly, patients with no pancreaticobiliary clinical symptoms and signs; secondly, patients with normal levels of pancreatic enzymes in the blood, urine, or other related biochemical indices; and thirdly, patients had a normal pancreas on MRI.
The inclusion criteria for the patients with acute pancreatitis (group B) involved the fulfillment of at least two of the following three criteria (13): (I) acute abdominal pain with the characteristics of acute pancreatitis; (II) increased levels of pancreatic enzymes and/or lipase in the blood, urine, or ascetic fluid (more than three times normal levels); and (III) abnormal imaging findings in the pancreas associated with acute pancreatitis. When a diagnosis is made on this basis, other pancreatic diseases and acute abdomen can be excluded. As exclusion criteria in this study, both groups excluded those patients with (I) chronic pancreatitis, pancreatic cancers, biliary tract neoplasms, ampullary carcinomas, and pancreatic and bile ducts located outside the duodenal wall, and group A excluded those with cholecystitis and biliary calculi; (II) poor image quality because of more ascites and artifacts; and (III) unclear and incomplete display of the common bile duct, pancreatic duct, and duodenal periampulla.
Finally, according to the inclusion and exclusion criteria, 72 patients were enrolled in this study. Group A had 32 subjects with normal pancreas; and group B had 40 patients with acute pancreatitis.
MR imaging techniques
The examination of the patients was performed on a 3.0 T superconducting scanner (MR750, GE Medical Systems, Waukesha, WI, USA) using a 32 channel phased-array abdominal coil for signal reception with respiratory gating and the patients laying in the supine position. The MRCP adopted a two-dimensional single shot fast spin-echo (SSFSE) by breath-hold. The imaging parameters for the SSFSE sequences were as follows: repetition time (TR)/echo time (TE) =6,000/900 ms; slice thickness (ST) =40 mm with no gap; FOV =38 cm, matrix =384×256 and scan time =3 seconds for one slice. The thick-slab sequences were acquired with a radial loop being centred at the level of the pancreaticobiliary junction. The first image of the radial loop was placed along the posterior border of the right hepatic lobe. The images were acquired during breath-hold at end expiration. Other sequences, such as the axial fast spoiled gradient echo (FSPGR) T1-weighted imaging with fat suppression, gradient-echo (GRE) T1-weighted in-phase and out-of-phase MR imaging, respiratory-triggered (R-T) axial fast recovery fast spin-echo (FRFSE) T2-weighted MR imaging with fat suppression, and coronal and axial SSFSE T2-weighted MR imaging were also performed as routine work.
Data measurement
We measured the APJ by applying the software of China Computer Aided Design (CCAD, China Shenzhen Jonathan Technology Co., Ltd). MRCP images were acquired and subsequently loaded in the digital imaging system and communications in medicine (DICOM) format. Then the DICOM format of images was input into the CCAD software, the radiologist measured the angle as follows (Figure 1). (I) The operator selected the MRCP images with a complete and clear display of the pancreatic duct, common bile duct and pancreaticobiliary junction; (II) the operator defined the initial region of interest (ROI) as a rectangle on the MRCP image, with the ROI including the pancreaticobiliary junction. The operator could adjust the ROI to fit the MRCP image, followed by magnifying the image to make the junction point between the common bile duct and pancreatic duct into the base point and drawing a line along the center of the pancreatic and common bile ducts with the mouse; (III) The radiologist measured the APJ based on the inflexion point of the pancreatic duct and common bile duct closest to the base point. The results were shown in the images automatically; (IV) the radiologist selected the largest angle image from these measured images, and then measured three times repeating the above steps on the selected image.

MR imaging interpretation and measurements
According to the type of biliary duct and main pancreatic duct joining the duodenal wall, the joining was classified into three categories: V type, B-P type and P-B type (14,15) (Figure 2). The V type is the pancreatic duct and biliary duct joining the duodenal wall without a common channel; the B-P type is the biliary duct draining into the pancreatic duct and forming a common channel; and the P-B type is the pancreatic duct draining into the biliary duct and forming a common channel.

The original MR imaging data were transferred to the CCAD software for review. Two radiologists selected a largest angle, completely displayed MRCP images together and then measured APJ on the same image independently. All MR imaging data were measured three times by the two radiologists independently using the same CCAD software.
Statistical analysis
Data are expressed as the mean ± standard deviation. Interobserver agreement was evaluated using intra-class correlation coefficient (ICC) statistics. The angles measured by the two observers between the two groups were compared by two independent sample t-tests. The comparison for the joining of the biliary duct and the main pancreatic duct among the three types (V type, B-P type and P-B type) was performed by the chi-square test and Fisher’s exact test for nominal data. The angles of the pancreaticobiliary junction with different types were compared by two independent sample t-tests. All these statistical tests were calculated using the Statistical Package for Social Sciences (SPSS) for Windows (Version 16.0, Chicago, IL, USA). P<0.05 was considered statistically significant.
Results
Patient sample
Group A included 16 women and 16 men with an average age of 52.31±15.45 years (range, 22-76 years). They were normal in 14 (43.8%) cases and had hepatic cysts in 7 (21.9%) cases, renal cysts in 5 (15.6%) cases, hepatic hemangiomas in 4 (12.5%) cases and splenic hemangiomas in 2 (6.2%) cases.
Group B included 19 women and 21 men with an average age of (50.38±10.15) years (range, 21-71 years). The causes for their pancreatitis included biliary calculi (40%, 16/40) and idiopathic (37.5%, 15/40). In addition, 7 (21.9%) patients had cholecystitis, and 2 (6.2%) patients had a cholecystectomy.
MRI findings
The quality of the MRI images in the 72 patients was good, clearly displaying the pancreas and its surrounding lesions. MRCP distinctly displayed the anatomy of the pancreaticobiliary junction, biliary calculi and dilatation of the bile and pancreatic ducts. Pancreatic variations or heterotopic pancreases were not found on the MRI.
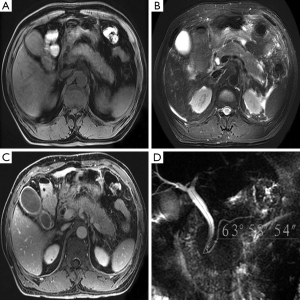
The interobserver agreement was excellent for the measurements of the APJ (ICC =0.988). APJ in all subjects was depicted very well on the MRCP (Figure 3).
In group A, 5 subjects (15.63%) had the V type, 8 (25%) had the B-P type, and 19 (59.37%) had the P-B type. In group B, 12 subjects (30%) had the V type, 18 (45%) had the B-P type, and 10 (25%) had the P-B type (Table 1). The prevalence of acute pancreatitis between the V type and P-B type and that between the B-P type and P-B type was significantly different (P=0.018 and P=0.01, respectively). The prevalence of acute pancreatitis in the V type (63.2%, 12/17) was higher than that in the P-B type (34.5%, 10/29), and the prevalence of acute pancreatitis in the B-P type (69.2%, 18/26) was also higher than that in the P-B type (34.5%, 10/29). The prevalence of acute pancreatitis between the V type and B-P type was not significantly different (P=0.925).
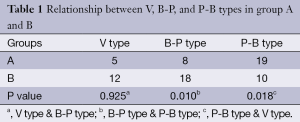
Full table
Relation between the APJ and acute pancreatitis
APJ in groups A and B was 51.45°±13.51° and 65.76°±15.61° respectively, with the later had a larger APJ (unpaired Student’s t-tests, P<0.001).
Relationship between the APJ and V type, B-P type and P-B type
There was no significant difference among the APJ of V type, B-P type and P-B type (P>0.05), with the average value being 59.32°±20.04°, 60.22°±11.06°, and 57.13°±17.27° respectively.
Discussion
Previous authors used compasses, vernier calipers and protractors to directly measure the angles on MRCP images or in cadaver specimens (7,16). In this study, we measured APJ on MRCP by CCAD in multiple orientations. Our study utilized image level with the maximum angle that completely displayed the bile common duct, pancreatic duct and pancreaticobiliary junction. In our results, the prevalence of acute pancreatitis was higher in the V and B-P types than in the P-B type. The P-B type involves the pancreatic duct draining into the biliary duct and forming a common channel. Studies (14,17) have revealed that the P-B type was equal to an acute angle and the B-P type was equal to a right angle. In this study APJ in non-pancreatitis subjects was smaller than those with acute pancreatitis. The reasons for this association may be that the increased APJ results in the pancreatic juice flowing more slowly into the duodenum and lead to potentially even inadequate drainage, which would then increase the pressure of the pancreatic duct or obstruction (8,18). Dysfunction of the major duodenal papilla ring sphincter and insufficiency of ampulla septum would increase the likelihood of pancreatic juice reflux (8,19). In addition, a large APJ may weaken the function of the pancreatic sphincter, which would lead to the reflux of bile juice and pancreatic juice (8,19). Therefore, the larger the APJ is, the steeper the bile duct is and the flatter the shape of the pancreatic duct is. On the other hand, acute pancreatitis results in edema of pancreatitis tissue in turn, which may change the APJ. In conclusion, this small scale study demonstrated the prevalence of acute pancreatitis was higher in the V and B-P types than in the P-B type, and a larger APJ was related to a higher prevalence of acute pancreatitis.
Acknowledgements
We thank Nan-Lin Zeng at our institution for providing the technical assistance of MRI.
Authors’ contributions: XH Huang, XM Zhang and GL Dong designed the research; N Liu, ZL Jing, CL Gao and MY Tang performed the research; N Liu, ZL Jing, CL Gao and MY Tang analyzed the data; N Liu and XH Huang wrote the paper.
Disclosure: The authors declare no conflict of interest.
References
- Chen Y, Zak Y, Hernandez-Boussard T, Park W, Visser BC. The epidemiology of idiopathic acute pancreatitis, analysis of the nationwide inpatient sample from 1998 to 2007. Pancreas 2013;42:1-5. [PubMed]
- Shen HN, Lu CL, Li CY. Epidemiology of first-attack acute pancreatitis in Taiwan from 2000 through 2009: a nationwide population-based study. Pancreas 2012;41:696-702. [PubMed]
- Bogdan J, Elsaftawy A, Kaczmarzyk J, Jabłecki J. Epidemiological characteristic of acute pancreatitis in Trzebnica district. Pol Przegl Chir 2012;84:70-5. [PubMed]
- Cruz-Santamaría DM, Taxonera C, Giner M. Update on pathogenesis and clinical management of acute pancreatitis. World J Gastrointest Pathophysiol 2012;3:60-70. [PubMed]
- Deng YY, Wang R, Wu H, Tang CW, Chen XZ. Etiology, clinical features and management of acute recurrent pancreatitis. J Dig Dis 2014;15:570-7. [PubMed]
- Gonoi W, Akai H, Hagiwara K, Akahane M, Hayashi N, Maeda E, Yoshikawa T, Kiryu S, Tada M, Uno K, Ohtsu H, Okura N, Koike K, Ohtomo K. Meandering main pancreatic duct as a relevant factor to the onset of idiopathic recurrent acute pancreatitis. PLoS One 2012;7:e37652. [PubMed]
- Ladas SD, Tassios PS, Giorgiotis K, Rokkas T, Theodosiou P, Raptis SA. Pancreatic duct width: its significance as a diagnostic criterion for pancreatic disease. Hepatogastroenterology 1993;40:52-5. [PubMed]
- Delhaye M, Matos C, Arvanitakis M, Deviere J. Pancreatic ductal system obstruction and acute recurrent pancreatitis. World J Gastroenterol 2008;14:1027-33. [PubMed]
- Bang S, Suh JH, Park BK, Park SW, Song SY, Chung JB. The relationship of anatomic variation of pancreatic ductal system and pancreaticobiliary diseases. Yonsei Med J 2006;47:243-8. [PubMed]
- Kamisawa T, Takuma K, Tabata T, Egawa N. Clinical implications of accessory pancreatic duct. World J Gastroenterol 2010;16:4499-503. [PubMed]
- Takuma K, Kamisawa T, Hara S, Tabata T, Kuruma S, Chiba K, Kuwata G, Fujiwara T, Egashira H, Koizumi K, Fujiwara J, Arakawa T, Momma K, Igarashi Y. Etiology of recurrent acute pancreatitis, with special emphasis on pancreaticobiliary malformation. Adv Med Sci 2012;57:244-50. [PubMed]
- Kamisawa T, Tu Y, Egawa N, Tsuruta K, Okamoto A, Kamata N. MRCP of congenital pancreaticobiliary malformation. Abdom Imaging 2007;32:129-33. [PubMed]
- Koizumi M, Takada T, Kawarada Y, Hirata K, Mayumi T, Yoshida M, Sekimoto M, Hirota M, Kimura Y, Takeda K, Isaji S, Otsuki M, Matsuno S. JPN. JPN Guidelines for the management of acute pancreatitis: diagnostic criteria for acute pancreatitis. J Hepatobiliary Pancreat Surg 2006;13:25-32. [PubMed]
- Todani T, Watanabe Y, Fujii T, Uemura S. Anomalous arrangement of the pancreatobiliary ductal system in patients with a choledochal cyst. Am J Surg 1984;147:672-6. [PubMed]
- Yamauchi S, Koga A, Matsumoto S, Tanaka M, Nakayama F. Anomalous junction of pancreaticobiliary duct without congenital choledochal cyst: a possible risk factor for gallbladder cancer. Am J Gastroenterol 1987;82:20-4. [PubMed]
- Park SW, Koh H, Oh JT, Han SJ, Kim S. Relationship between Anomalous Pancreaticobiliary Ductal Union and Pathologic Inflammation of Bile Duct in Choledochal Cyst. Pediatr Gastroenterol Hepatol Nutr 2014;17:170-7. [PubMed]
- Komi N, Takehara H, Kunitomo K, Miyoshi Y, Yagi T. Does the type of anomalous arrangement of pancreaticobiliary ducts influence the surgery and prognosis of choledochal cyst? J Pediatr Surg 1992;27:728-31. [PubMed]
- Arendt T. Bile-induced acute pancreatitis in cats. Roles of bile, bacteria, and pancreatic duct pressure. Dig Dis Sci 1993;38:39-44. [PubMed]
- Kamisawa T, Okamoto A. Biliopancreatic and pancreatobiliary refluxes in cases with and without pancreaticobiliary maljunction: diagnosis and clinical implications. Digestion 2006;73:228-36. [PubMed]


