New vistas in clinical practice: susceptibility-weighted imaging
Introduction
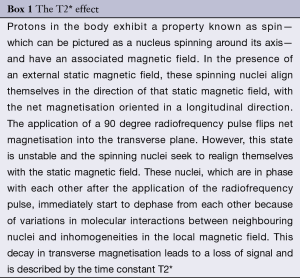
Susceptibility-weighted imaging (SWI) is a relatively recently developed magnetic resonance imaging (MRI) technique where the image contrast is mainly based on ‘magnetic susceptibility effects’—a natural property of tissues. This property reflects the magnetic response of a substance to an external magnetic field. The difference in susceptibility between substances leads to local magnetic field inhomogeneities, which results in faster T2* relaxation (Box 1), leading to signal loss on MR sequences sensitive to T2* effects (1). Substances that exhibit a strong susceptibility effect are more easily detected using SWI. Examples of substances that have a strong susceptibility effect include ferromagnetic substances such as iron, paramagnetic substances including blood products and gadolinium (MR contrast agent) and diamagnetic substances such as calcium.
Full table
The SWI technique (Box 2)
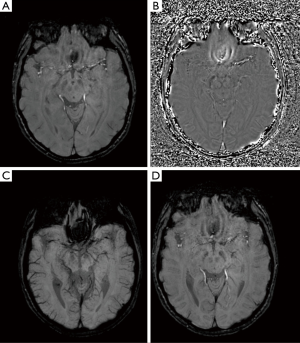
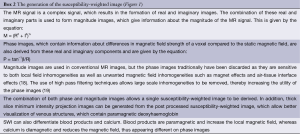
SWI employs a high resolution 3D gradient-recalled echo sequence with a long echo time and flow compensation, utilising both magnitude and phase information (1), which allows for increased sensitivity in the detection of susceptibility effects.
The phase information contains important information about differences in magnetic field strength in a particular MR voxel. As such the combination of both the phase and magnitude images into a single susceptibility-weighted image are of greater utility than magnitude images alone, for example in identifying blood products (2).
An added advantage of SWI over the current gradient echo sequences is the ability to differentiate between blood products and calcification or mineralization (3) (Figure 2).
Clinical applications of SWI
The applications of SWI are rapidly increasing, with much work being carried out to determine the usefulness of the technique in multiple disease states.
Cerebral microbleeds (CMBs)
The most common application of SWI currently is in the detection of CMBs. These are small rounded homogeneous foci of low signal on gradient echo sequences (4), which correlate histopathologically with blood-breakdown products (5). CMBs are commonly seen in the elderly population and tend to increase with age, affecting more than 40% of people over 80 (6).
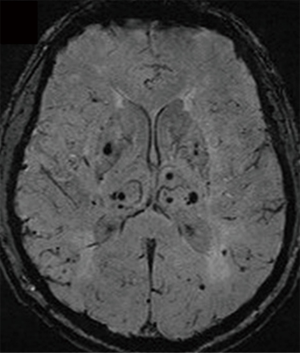
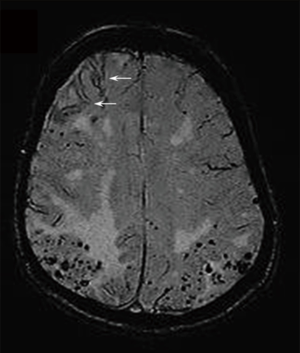
CMBs are mainly associated with two forms of small vessel disease: hypertensive arteriopathy and cerebral amyloid angiopathy (CAA), the latter which is found commonly in Alzheimer’s disease, dementia and ageing. SWI can be used to differentiate between these two forms based on the topographical distribution of CMBs. In hypertensive arteriopathy, the CMB distribution tends to be in the basal ganglia, thalamus and brainstem (Figure 3). In contrast, the CMBs in CAA tend to occur in a lobar distribution and at the grey-white matter interface (7) (Figure 4). SWI may further assist in identifying the presence of haemosiderin deposition and convexity subarachnoid hemorrhage (SAH), which are further identifying features of CAA (Figure 4).
The identification of CMBs in specific treatment settings is also of value in determining future risk of intracerebral hemorrhage (ICH). The presence of CMBs in patients treated with warfarin or antithrombotic drugs are at increased risk of ICH (8).
Neurodegeneration
The sensitivity of SWI to ferromagnetic substances makes it an appropriate tool to assess brain iron content (9). Elevated iron content is demonstrated in many neurodegenerative disorders including Parkinson’s disease, Alzheimer’s disease and Huntington’s disease. In addition, iron accumulation in the basal ganglia is also seen in neurodegeneration with brain iron accumulation, a heterogeneous group of genetic extrapyramidal motor disorders that typically present at an early age.
Stroke
The use of SWI in the imaging of acute stroke may serve several purposes. By identifying underlying CMBs, it may be possible to predict the risk of developing an ICH after thrombolysis (10), as well as identifying areas of hemorrhage within an infarct (11). In addition, SWI may be useful in identifying intravascular thrombus during the acute event (12).
Intracerebral tumours
SWI may be used to better characterize brain tumors, particularly in relation to the internal architecture and areas of calcification and/or intratumoral hemorrhage. This can provide additional information about the grading of a particular tumor (9).
Subarachnoid hemorrhage (SAH)
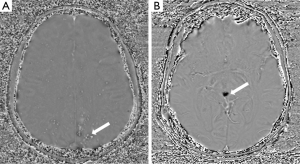
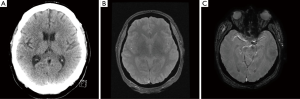
SWI has been utilized in the diagnosis of spontaneous cortical SAH (13,14) and as a diagnostic aid to localize the source of bleeding in patients with multiple cerebral aneurysms (15). SWI also appears to provide enhanced detection of traumatic SAH compared to CT (16). Our experience also indicates that SWI can identify spontaneous SAH in cases where the initial CT is negative (see Figure 5) supporting the findings of Verma et al., 2013 (17). Further study is warranted to evaluate the effectiveness of the technique in this setting.
Conclusions
SWI has been shown to be useful in the investigation of multiple disease states, particularly in neurovascular and neurodegenerative disorders. As such, this technique has becoming increasingly incorporated into routine MR neuroimaging protocols.
Disclosure: The authors declare no conflict of interest.
References
- Haacke EM, Mittal S, Wu Z, Neelavalli J, Cheng YC. Susceptibility-weighted imaging: technical aspects and clinical applications, part 1. AJNR Am J Neuroradiol 2009;30:19-30. [PubMed]
- Ayaz M, Boikov AS, Haacke EM, Kido DK, Kirsch WM. Imaging cerebral microbleeds using susceptibility weighted imaging: one step toward detecting vascular dementia. J Magn Reson Imaging 2010;31:142-8. [PubMed]
- Wu Z, Mittal S, Kish K, Yu Y, Hu J, Haacke EM. Identification of calcification with MRI using susceptibility-weighted imaging: a case study. J Magn Reson Imaging 2009;29:177-82. [PubMed]
- Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, Launer LJ, Van Buchem MA, Breteler MM; Microbleed Study Group. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 2009;8:165-74. [PubMed]
- Fazekas F, Kleinert R, Roob G, Kleinert G, Kapeller P, Schmidt R, Hartung HP. Histopathologic analysis of foci of signal loss on gradient-echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: evidence of microangiopathy-related microbleeds. AJNR Am J Neuroradiol 1999;20:637-42. [PubMed]
- Poels MM, Vernooij MW, Ikram MA, Hofman A, Krestin GP, van der Lugt A, Breteler MM. Prevalence and risk factors of cerebral microbleeds: an update of the Rotterdam scan study. Stroke 2010;41:S103-6. [PubMed]
- Vernooij MW, van der Lugt A, Ikram MA, Wielopolski PA, Niessen WJ, Hofman A, Krestin GP, Breteler MM. Prevalence and risk factors of cerebral microbleeds: the Rotterdam Scan Study. Neurology 2008;70:1208-14. [PubMed]
- Lovelock CE, Cordonnier C, Naka H, Al-Shahi Salman R, Sudlow CL; Edinburgh Stroke Study Group, Sorimachi T, Werring DJ, Gregoire SM, Imaizumi T, Lee SH, Briley D, Rothwell PM. Antithrombotic drug use, cerebral microbleeds, and intracerebral hemorrhage: a systematic review of published and unpublished studies. Stroke 2010;41:1222-8.
- Mittal S, Wu Z, Neelavalli J, Haacke EM. Susceptibility-weighted imaging: technical aspects and clinical applications, part 2. AJNR Am J Neuroradiol 2009;30:232-52. [PubMed]
- Charidimou A, Kakar P, Fox Z, Werring DJ. Cerebral microbleeds and the risk of intracerebral haemorrhage after thrombolysis for acute ischaemic stroke: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2013;84:277-80. [PubMed]
- Wycliffe ND, Choe J, Holshouser B, Oyoyo UE, Haacke EM, Kido DK. Reliability in detection of hemorrhage in acute stroke by a new three-dimensional gradient recalled echo susceptibility-weighted imaging technique compared to computed tomography: a retrospective study. J Magn Reson Imaging 2004;20:372-7. [PubMed]
- Santhosh K, Kesavadas C, Thomas B, Gupta AK, Thamburaj K, Kapilamoorthy TR. Susceptibility weighted imaging: a new tool in magnetic resonance imaging of stroke. Clin Radiol 2009;64:74-83. [PubMed]
- Field DK, Kleinig TJ. Aura attacks from acute convexity subarachnoid haemorrhage not due to cerebral amyloid angiopathy. Cephalalgia 2011;31:368-71. [PubMed]
- Cuvinciuc V, Viguier A, Calviere L, Raposo N, Larrue V, Cognard C, Bonneville F. Isolated acute nontraumatic cortical subarachnoid hemorrhage. AJNR Am J Neuroradiol 2010;31:1355-62. [PubMed]
- Kheĭreddin AS, Pronin IN, Kornienko VN, Belousova OB. Diagnosis of the source of bleeding in multiple cerebral aneurysms by susceptibility-weighted imaging. Vestn Rentgenol Radiol 2012;4-9. [PubMed]
- Wu Z, Li S, Lei J, An D, Haacke EM. Evaluation of traumatic subarachnoid hemorrhage using susceptibility-weighted imaging. AJNR Am J Neuroradiol 2010;31:1302-10. [PubMed]
- Verma RK, Kottke R, Andereggen L, Weisstanner C, Zubler C, Gralla J, Kiefer C, Slotboom J, Wiest R, Schroth G, Ozdoba C, El-Koussy M. Detecting subarachnoid hemorrhage: comparison of combined FLAIR/SWI versus CT. Eur J Radiol 2013;82:1539-45. [PubMed]
- Haacke EM, Boikov AS, Barnes E, Neelavalli J, Khan MA. Susceptibility-weighted imaging. In: Werring DJ. eds. Cerebral Microbleeds: Pathophysiology to Clinical Practice. Cambridge University Press, 2011:22-33.
- Haacke EM, Xu Y, Cheng YC, Reichenbach JR. Susceptibility weighted imaging (SWI). Magn Reson Med 2004;52:612-8. [PubMed]