Conversations in the operating room: history of the development of a promising new compound for the treatment of premature ejaculation
“It would be a mistake to rely on drugs alone for restoration of so complex a function” - B. Schapiro, 1943 (1)
Despite its large prevalence (2,3) Premature Ejaculation (PE) remains incompletely understood; consequently, its treatment is diverse and frequently non-specific (4). Over the years, many sundry approaches have been used. In the days of Freudian theory, PE was thought to result from unresolved narcissism or an unconscious, deep-seated hatred of women (5) PE has long been considered a learned behavior with a significant psychological component, thus psychosexual therapies that combine behavioral interventions and counseling to lessen performance anxiety remain widely used, despite limited and temporary success. The serendipitous finding that delayed ejaculation is a common side effect of psychotropic or anti-depressant drugs resulted in their extensive use for treatment of PE. At first tricyclic anti-depressants (clomipramine) were put to this use; later followed on with serotonin reuptake inhibitors (SSRIs) (6), most commonly fluoxetine, paroxetine and sertraline.
The current neurobiological explanation for PE advances the concept that serotonin and its receptors are the primary control mechanism of the ejaculatory reflex. Documented in animal models, these concepts are postulated as the rationale for the response to SSRIs in humans (7). The efficacy and safety of SSRIs, however, leaves much room for improvement. A more recent SSRI, dapoxetine, has been approved in a few countries and is widely advertised in the internet. But it has provoked significant controversy (8,9) and has received a “letter of not approval” from the FDA despite several controlled clinical trials (10).
A different approach to control the ejaculatory reflex aims to decrease afferent signaling by blocking the sensitive fibers with the use of topical anesthetic agents. The rationale here is that reducing the sensitivity of the glans penis, would result in a delay in intra-vaginal latency time (IVELT) without affecting the sensation of ejaculation. The concept of local therapy was first reported by Schapiro (1) more than 60 years ago. In a paper remarkably short on detail, he reported his large experience in pre-war Germany in patients with PE whom he claimed to have treated with topical camphor, belladonna and the opium alkaloid stypticine for an astonishing 82% response rate. In keeping with contemporary reporting styles, little information was provided as to the criteria for diagnosis and response, or the methodology used. Perhaps the paucity of details contributed to the total silence on this avenue of treatment for PE during the next 3 decades. The lack of interest is surprising since topical agents offer several advantages: they can be used on “as needed” basis and their systemic effects are minimal. Their two major drawbacks are the possibility of global penile hypoesthesia and the risk of transvaginal contamination resulting in vaginal anesthesia.
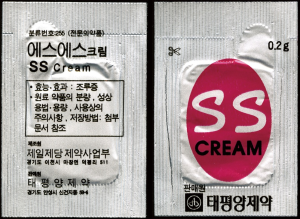
The resurgence of topical therapy for PE occurred at the 6th World Meeting on Impotence in Singapore in 1994 by Xing et al. (11) on the use of a preparation named SS-cream (Figure 1). Formal results of the clinical trial were published 5 years later (12). This experience was in keeping with a rekindled interest in new delivery forms of topical anesthetics in general (13).
The name, SS-cream, derives from the institution where it was developed (Seoul Severance Hospital). It contains “carefully selected extracts of nine natural products… (which) are believed to have local desensitizing effects…”. The cream was reported to be free of significant adverse effects except for a mild burning sensation (15% vs. 7% in the placebo group). Efficacy was dose-dependent (from 0.05 to 0.2 gms): 84% of patients experienced an increase in IVELT of >2 min. with the highest dose; only 30% responded to the lowest dose and 18% to placebo. Despite the appealing results, the drug does not appear to have been used outside the Korean peninsula and the prospects of gaining regulatory approval seem very slim.
A different approach involved the topical anesthetic diclonine mixed with prostaglandin E1 in a cream to be applied to the meatus (14). Again a dose response was observed, using the criterion of an increase of >2 minutes in IVELT, ranging from 66.7% for the placebo group to 86.7% for the higher dose of the active compound. To our knowledge a formal paper of this study has not been published.
The idea of topical anesthetics is enduring and appealing. The internet is crawling with hyperbolic claims of useless “cures” having no credible evidence of efficacy. A number of over-the-counter agents are available (e.g., lidocaine 9.6% spray), but adequate clinical studies are lacking. The one exception is the combination lidocaine-prilocaine. These two drugs are crystalline solids that, when mixed together, form a liquid (eutectic) mixture that can be formulated into a preparation that allows higher drug delivery. The eutectic mixture is commercialized by AstraZeneca as a topical anesthetic under the name EMLA, containing 2.5% each of lidocaine/prilocaine for application to intact skin.
The initial experience using this cream, by Berkovitch et al. (15), consisted of an open-label study of 11 patients who applied the cream to the glans and shaft of the penis 30 minutes prior to intercourse. The results were rated as “better” or “excellent” by 9 of the 11 patients and all partners were satisfied with the results. A placebo controlled study of 10 patients, which was aimed at optimizing treatment with EMLA, found that IVELT increased in all patients using the active compound. However, those with a residence time for the cream of 45 minutes or more experienced not only penile numbness but erectile difficulties. The authors concluded that the optimum penile residence time was 20 minutes (16).
Interest in EMLA for PE persisted and a larger, double-blind, controlled trial was launched: patients applied cream to the glans and distal 2 cm of the penile shaft and covered the area with a condom, “to avoid losing the cream” for 10-20 minutes prior to intercourse (17). The results demonstrated an almost 6-fold increase in IVELT, although only 69% of the patients completed the study. Adverse effects occurred in 17% of those using EMLA and none in the placebo group.
A further refinement was offered by Metin et al. (18) who treated PE with fluoxetine on an “as per needed” basis to be taken 4 hours prior to intercourse for 3 months and then added lidocaine cream 30 min before sexual activity for another 3 months. According to a grading scale developed by the authors, there was a remarkable improvement of 86.9% at the end of the whole trial.
Topical anesthetics are easily obtainable for a variety of indications (from sunburns to minor scrapes and lacerations) and men have been applying them to their penises as a treatment for PE or for recreational purposes for a long time.
The lidocaine-prilocaine spray (LPS) eureka moment
During his residency training program in Anesthesia at Queen’s University in Canada (1991 to 1994), Richard Henry was instructed on the technique of intubation for induction of anesthesia. It was common practice in those days to use topical anesthesia to blunt the laryngeal spasms resulting from the stress response to intubation with a topical aerosol application. At the time, lidocaine was delivered by suspending the insoluble particles of the drug in liquid propellants in a pressurized container. Environmental concerns expressed in the Montreal Protocol (19) banned their use and promoted the switch to hydrofluorocarbon propellants. These, however, exhibit poor solubility characteristics; newer techniques relied on dissolving the anesthetic agent in ethanol and then dissolving the solution into the propellant. The new systems were suitable for delivery of bronchodilators that require small dosage (100-200 micrograms per metered dose) but were wholly inappropriate for topical anesthetics requiring much higher concentrations (10 mg per metered dose). After much experimentation and technical help initially from Astra Canada (Toronto, Ontario) and later on from Charles Eck of DuPont (Wilmington, Delaware), a small group of researchers, led by Richard Henry, huddled in Eck’s laboratory and delivered 5 grams of lidocaine base into a glass aerosol bottle, capped and pressure injected 10 cc of HFC1234 propellant. There was an audible gasp when the white lidocaine powder disappeared like magic into solution. The remarkable event led Eck’s facility to produce a few canisters of lidocaine base aerosol –10 mg per actuation for further human experimentation (Figure 2). This pioneering work revealed: (I) no effect on intact skin, (II) excellent numbing of the upper respiratory tract (appropriated for airway anesthesia, intubation, brochoscopy), (III) nasal anesthesia and (IV) anesthesia of the glans penis (as a potential agent circumcision).
Topical delivery of lidocaine remained the biggest obstacle until Henry found that the eutectic mixture of lidocaine and prilocaine was equally soluble in HFC propellants and that prilocaine interacted with the propellant to enhance the solubility of other drugs. This observation was unexpected and constituted the bases of granting Henry US patent number 5,858,331 on January 12, 1999. Despite the impressive performance of LPS, pharmaceutical corporations could see no clinical potential and refused options for its commercialization.
The human observations, described informally by Henry at clinical rounds and in the operating room piqued the interest of the author, a urologist, who saw the obvious promise of the spray in men with PE. Through mutual interest and collaboration, an open label (proof-of-concept) study was carried out on a limited number of couples affected with PE (n=14). For the study, a metered-dose canister delivered a mixture of 7.5 mg of lidocaine base and 2.5 mg of prilocaine base per actuation. Male subjects were to apply 3-5 actuations directly into the glans (depending on size) and to remove with a damp cloth after 15 min. The 11 patients who completed the study, documented by stop watch a significant increase in IVELT (from 1 min: 24 s at baseline to 11 min: 21 s, P=0.008). There was also an improvement in overall satisfaction. Numbness was reported by 2 men but it did not affect the quality of the orgasm (20).
Phase II studies on LPS were carried out initially in Europe (21). The combination was found to produce a significant benefit in inducing delayed ejaculation with minimal adverse effects.
Using a more elaborate canister (Figure 3) for delivery, the compound was evaluated in 2 multicenter, double-blind, randomized trials one in several European countries (22) and almost simultaneously, another one in Canada, the United States and Poland (23). In all 3 studies the drug produced a significant benefit by increasing the geometric mean of IVELT from 0.56 min to 2.60 min during the 3 months duration of the study. The majority of patients (52%) rated the response good/excellent in the treatment group while <10% did so in the placebo cohort. Adverse effects were few and included loss of erection and general erythema in <5%. Partner related undesirable effects included vulvo-vaginal burning and discomfort in <10%.
Having completed the process of clinical evaluation starting with a proof-of-concept study and culminating with 2 international, multicenter phase III trials in Europe and North America, the future commercialization of LPS rest now on the ability of industry to obtain approval from Health Canada, the Food and Drug Administration in the United States and the European Medicines Agency.
In conclusion, the development of a compound intended to facilitate intubation of the upper respiratory tract and the performance of circumcisions, particularly in neonates, has found its most relevant application in the improvement of PE. All of this thanks to the exchange of ideas between specialists in the operation theatre.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Schapiro B. Premature ejaculation, a review of 1130 cases. J Urol 1943;50:374-9.
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44. [PubMed]
- Dean J. The European online sexual survey (EOSS): Pan-European perspectives on the impact of premature ejaculation and treatment-seeking behavior. Eur Urol 2007;6:768-74.
- Shindel A, Nelson C, Brandes S. Urologist practice patterns in the management of premature ejaculation: a nationwide survey. J Sex Med 2008;5:199-205. [PubMed]
- Ellis H. eds. Studies in the Psychology of Sex. New York: Random House, 1936.
- Waldinger MD. The neurobiological approach to premature ejaculation. J Urol 2002;168:2359-67. [PubMed]
- Waldinger MD, Berendsen HH, Blok BF, et al. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: the involvement of the serotonergic system. Behav Brain Res 1998;92:111-8. [PubMed]
- Goldstein I. Regarding Waldinger and Schweitzer’s “premature ejaculation and pharmaceutical company-based medicine: the dapoxetine case”. J Sex Med 2008;5:965. [PubMed]
- Waldinger MD, Schweitzer DH. Premature ejaculation and pharmaceutical company-based medicine: the dapoxetine case. J Sex Med 2008;5:966-97. [PubMed]
- McMahon C, Kim SW, Park NC, et al. Treatment of premature ejaculation in the Asia-Pacific region: results from a phase III double-blind, parallel-group study of dapoxetine. J Sex Med 2010;7:256-68. [PubMed]
- Xin ZC, Seong DH, Minn YG, et al. A Double Blind Clinical Trial of SS-cream on Premature Ejaculation. Korean J Urol 1994;35:533-7.
- Choi HK, Xin ZC, Choi YD, et al. Safety and efficacy study with various doses of SS-cream in patients with premature ejaculation in a double-blind, randomized, placebo controlled clinical study. Int J Impot Res 1999;11:261-4. [PubMed]
- Henry R, Morales A, Wyllie MG. TEMPE: Topical Eutectic-Like Mixture for Premature Ejaculation. Expert Opin Drug Deliv 2008;5:251-61. [PubMed]
- Gittelman M, Mo J, Lu M. Synergistic effect of meatal application of dyclonin/alprostadil cream for the treatment of early ejaculation (EE) in a double blind and cross-over study. J Sex Med 2006;3:230.
- Berkovitch M, Keresteci AG, Koren G. Efficacy of prilocaine-lidocaine cream in the treatment of premature ejaculation. J Urol 1995;154:1360-1. [PubMed]
- Atikeler MK, Gecit I, Senol FA. Optimum usage of prilocaine-lidocaine cream in premature ejaculation. Andrologia 2002;34:356-9. [PubMed]
- Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: a double-blind, randomized, placebo-controlled study. BJU Int 2004;93:1018-21. [PubMed]
- Metin A, Kayigil O, Ahmed SI. Does lidocaine ointment addition increase fluoxetine efficacy in the same group of patients with premature ejaculation? Urol Int 2005;75:231-4. [PubMed]
- Available online: http://ozone.unep.org/Ratification_status/
- Henry R, Morales A. Topical lidocaine-prilocaine spray for the treatment of premature ejaculation: a proof of concept study. Int J Impot Res 2003;15:277-81. [PubMed]
- Dinsmore WW, Hackett G, Goldmeier D, et al. Topical eutectic mixture for premature ejaculation (TEMPE): a novel aerosol-delivery form of lidocaine-prilocaine for treating premature ejaculation. BJU Int 2007;99:369-75. [PubMed]
- Dinsmore WW, Wyllie MG. PSD502 improves ejaculatory latency, control and sexual satisfaction when applied topically 5 min before intercourse in men with premature ejaculation: results of a phase III, multicentre, double-blind, placebo-controlled study. BJU Int 2009;103:940-9. [PubMed]
- Carson C, Wyllie M. Improved ejaculatory latency, control and sexual satisfaction when PSD502 is applied topically in men with premature ejaculation: results of a phase III, double-blind, placebo-controlled study. J Sex Med 2010;7:3179-89. [PubMed]