The science of vacuum erectile device in penile rehabilitation after radical prostatectomy
Introduction
Prostate cancer is the most common solid organ cancer in men and is ranked second as a cause of death in America (1). Radical prostatectomy (RP) is a standard surgical treatment for clinically localized prostate cancer (2). However, erectile dysfunction (ED) following prostatectomy remains a significant quality of life issue for men undergoing prostatectomy. It is estimated to affect 26-100% of patients after surgery (3). Penile shrinkage after RP is another common issue. It was documented that penile length shortening occurs in 68% to 71% of men undergoing RP (4) and is usually accompanied by ED (5).
Fraiman et al. conducted research which included 100 ED patients after nerve-sparing radical retropubic prostatectomy (NSRRP) and reported that there was a significant decrease in penile size in men with ED after NSRRP. The flaccid and erect measurements of length and circumference decreased 8% and 9%, respectively after surgery. The most substantial change occurred between the first 4 and 8 months postoperatively (6). Munding et al. showed that the stretched penile length decreases after RP at 3 months follow-up in 22/31 patients; 48% had considerable shortening greater than 1.0 cm (7). Savoie et al. studied 124 men and evaluated penile length before and 3 months after RP in a prospective study and found significant decrease in the flaccid, stretched and circumferential measurements of the penis at 3 months (8).
Penile rehabilitation post RP is widely applied in clinical practice to improve patient quality of life (9,10). Penile rehabilitation methods include the use of phosphodiesterase type 5 inhibitors (PDE5i), the vacuum erectile device (VED), intracavernosal injection/intraurethral suppository, or combination therapy (9). Current studies show that VED therapy plays an important role in penile rehabilitation post RP. Teloken et al. took a survey of 301 physicians from 41 countries, who were members of the International Society for Sexual Medicine (ISSM) in 2009. 83.7% of the physicians performed penile rehabilitation post RP. The rehabilitation strategies were: PDE5i 95.4%; ICI 75.2%; VED 30.2%; MUSE 9.9% (11). Another survey was conducted during the American Urological Association (AUA) annual meeting in 2011 which included 618 urologists. The study showed that 85.8% of them performed penile rehabilitation after RP and VED has become the second most commonly used method (12).
VED uses negative pressure to distend the corporal sinusoids and to increase blood inflow to the penis (13). Depending on its purpose, VED could be used with the aid of an external constricting ring which is placed at the base of penis to prevent blood outflow, maintaining the erection for sexual intercourse. Also, VED could be used without the application of a constriction ring, just to increase blood oxygenation to the corpora cavernosa (14). This direct artificial erection can circumvent the limitation of oral agents, which requires intact and functioning cavernosal nerves to produce erections. This can be a significant factor even in men undergoing bilateral nerve sparing RP, as neuropraxia still occurs and can diminish the effectiveness of PDE5i (15). VED therapy has the additional benefit of being non-invasive, and more cost-effective with lower risk for systemic side effects than other alternatives for penile rehabilitation (14,16).
However, the underlying mechanisms of VED therapy are still unclear. This paper is designed to review the scientific evidences of VED therapy post RP and discuss the possible mechanisms.
Mechanisms of ED post radical prostatectomy
Erectile function impaired immediately following RP is thought to be due to the damage to the cavernous nerves, which is known as neuropraxia (17). Neuropraxia can be caused by mechanically induced nerve stretching that may occur during prostate retraction, thermal damage to the nerve caused by electrocautery, ischemia of the nerves secondary to disruption of blood supply while attempting to control surgical bleeding, and local inflammatory effects associated with surgical trauma (17). Even in the most meticulous nerve-sparing dissection, some degree of neuropraxia is unavoidable because of the close proximity of the nerves to the prostate gland. These nerves tend to recover slowly; it may take as long as 18-24 months for them to reach a new baseline functional status (18). Absence or decreased erection with loss of penile size ensues before recovery of the cavernous nerve (6,19).
Lack of erections will then lead to poor oxygenation of the corporal bodies, eventually progressing to cavernosal fibrosis, and ultimately causing a venous leak seen clinically as venogenic ED (20). In an experimental model, significant over-expression of hypoxia-related substances, such as Hypoxia-inducible factor (HIF-1-α) and transforming growth factor beta-1 (TGF-β1), were found in rats that had undergone bilateral excision of the cavernosal nerves compared with controls (21). When human penile smooth muscle cell is exposed to a prolonged hypoxic environment, TGF-β1 dependent endothelin-1 (ET-1) synthesis is increased. ET-1 is a potent constrictor of penile smooth muscle and a profibrotic peptide (22). Studies also showed that low oxygen tension in human cavernosal tissue inhibits production of prostaglandin-E1 (PGE1). PGE1 inhibits collagen formation by inhibiting TGF-β1 which induces collagen synthesis. With the inhibition of PGE1, TGF-β1 is allowed to induce connective tissue synthesis (20). The trabecular smooth muscle is then replaced with collagen, which leads to the loss of the veno-occlusive mechanism (23,24).
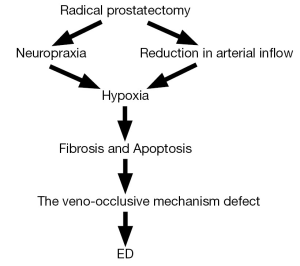
A reduction in arterial inflow was also reported by several authors. This is associated with the ligation of accessory internal pudendal arteries during prostatectomy (25,26). Combination of nerve damage with decreased arterial inflow may intensify hypoxia and ultimately lead to apoptosis which is an underlying cause of post RP induced ED. User et al. performed bilateral neurotomy of the rat penis and found that there was significant apoptosis in the subalbugineal smooth muscle cells. With apoptosis in the region of the subtunical venular plexus, a defect in the veno-occlusive mechanism of the corpus cavernosum occurs (27). McVary et al. recently confirmed that a 12-fold increase of apoptosis happened in penile smooth muscle in rats whose cavernous nerves were disrupted (28).The current understanding of ED after RP is summarized in Figure 1.
Mechanisms of penile shrinkage after radical prostatectomy
The mechanisms of penile shortening are unclear. The most common explanation given by urologists to patients is that the extirpation of the prostate results in shortening of the urethra by several centimeters, which results in penile shortening. However, this explanation was criticized as having no scientific foundation (29). User et al. reported penile wet weight and DNA content were significantly decreased at each time point after bilateral cavernous nerve transection in an animal study. They suggested that the penile wet weight loss and DNA content decrease related to the apoptotic mechanisms (30). There are some commonly accepted theories including cavernosal nerve injury induced denervation structural alterations, hypoxia related ultra-structural changes in penis and sympathetic hyper-innervation (16,29).
Science of VED therapy after RP
Clinical evidence
Zippe et al. confirmed the safety and tolerability of VED use as rehabilitation for patients after RP (31,32). Studies have shown that VED therapy improves erectile function in 84-95% of patients (16,31,33,34). Raina et al. found 17% vs. 11% recovery of erectile function with daily use of VED compared to non-VED use; and only 23% VED users vs. 85% non-VED users reported penile shrinkage in a 9-month study with total of 109 patients who underwent nerve-sparing or non-nerve-sparing RP (35).
It is suggested that penile rehabilitation with VED should began early after RP. Köhler et al. found early use of VED (1 month after RP) improved sexual function recovery and helped the preservation of penile length. In their study, 28 men undergoing RP were randomized to early intervention (1 month after RP, group 1), or a control group (6 months after RP, group 2) using a traditional VED protocol (10 minutes of VED usage without the constriction band). International Index of Erectile Function (IIEF) questionnaire and penile length data were collected at baseline, 1, 3, 6, 9, and 12 months. The mean follow-up was 9.5 months. The IIEF scores were significantly higher in group 1 than group 2 at 3, 6 months after RP. Compared to group 1, Stretched penile length was significantly decreased at both 3 and 6 months, by approximately 2 cm in group 2 (16). Dalkin et al. also strongly recommended early intervention with the daily use of VED after RP. In their study, 42 men who underwent nerve-sparing RP had penile measurements before surgery and 3 months after surgery by a single investigator to evaluate penile shortening. Daily use of VED was begun at the day after catheter removal, and continued for 90 days. Penile shortening ≥1.0 cm was considered significant. 39 of 42 men completed the study. In men who complied well with VED therapy, only 1/36 (3%) had a decrease of penile length ≥1.0 cm. Of the three men with poor VED compliance, two (67%) had a reduction in penile length ≥1.0 cm. Compared to prior studies where 48% of men after surgery had a significant reduction in penile length, early intervention with the daily use of a VED resulted in a significantly lower risk of loss of penile length (36).
Animal study
To understand the mechanism of VED in penile rehabilitation, we designed a rat specific VED based on the principle of human VED (13). An underlying mechanism exploratory study was carried out on rats with bilateral cavernous nerve crush (BCNC) model. Sprague-Dawley (SD) rats were randomly assigned into three groups: sham, BCNC, and BCNC plus VED. VED therapy began 2 weeks after BCNC surgery, 5 mins twice daily from Monday to Friday for 4 weeks. The study showed that VED therapy could decrease the HIF-1a, TGF-β1 and Terminal deoxynucleotidyl transferase biotin-dUTP nick end labeling (TUNEL) expression and increase Intracavernous Pressure/Mean Arterial Pressure (ICP/MAP), endothelial nitric oxide synthase (eNOS), alpha smooth muscle actin (α-SMA) and masson’s trichrome (MT) expression in BCNC rat model. This study first demonstrated the effectiveness of VED therapy on ED in the nerve injury rat model. The beneficial effect of VED therapy may relate to anti-hypoxia, anti-fibrosis and anti-apoptosis mechanisms (37). A further study was performed to estimate the effect of VED therapy on penile length and cavernous oxygen saturation (SO2) in the BCNC rat model. Penile length and diameter were measured on a weekly basis. After 4 weeks of therapy, penile blood was extracted by three methods for blood gas analysis: Method 1, cavernous blood was aspirated at the flaccid state; Method 2, cavernous blood was aspirated at the traction state; Method 3, cavernous blood was aspirated immediately after applying VED. SO2 values were tested by the blood gas analyzer. Our unpublished data showed that VED therapy is effective in preventing penile shrinkage induced by BCNC. Also, the penile SO2 was increased by VED application compared to flaccid or traction groups. The calculated blood constructs in corpus cavernosum right after VED application were more arterial blood than venous blood. This study further suggests that VED therapy can effectively preserve penile size in the cavernous nerve injury animal model. This study also provided the direct basic scientific evidence that VED therapy increases arterial inflow.
The possible mechanisms of VED on treating ED post RP
There are overlapping mechanisms of ED and penile shrinkage after RP. Reduced erection and arterial inflow with hypoxia are the main contributors of both ED and penile shrinkage after RP. The tissue hypoxia and structure change play a key role in the progression of the disease. VED therapy targets this pathology pathway. Physiologically, the VED uses negative pressure to distend the corporal sinusoids and to increase blood inflow into the penis (13), which causes penile passive engorgement. Bosshardt et al. confirmed that there is a passive congestion of mixed arterial and venous blood, with extra-tunica tissue making up a large component of the increased diameter. Their data showed that mean SO2 of corporeal blood immediately after VED induced erection was 79.2% in the patient. 58% of blood with VED induced erection was arterial and 42% of blood was venous in origin (38). Our animal study confirmed their findings and suggested VED application increases the arterial blood inflow to the penis to reverse the hypoxia process.
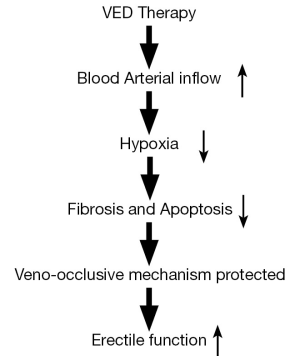
Riana et al. suggested that the use of the VED helped to inhibit abnormal collagen or scar formation in the hypoxic penile conditions after RP (35). The increased arterial inflow in the penis increased tissue oxygen levels, which effectively alleviated the tissue hypoxia damage caused by cavernous nerve injury. This may also inhibit the tissue cell apoptosis and prevent the cavernosal tissue fibrosis. As shown in our previous study (37), the VED can prevent penile tissue apoptosis (TUNEL) and fibrosis (TGF-β1). The smooth muscle (α-SMA, MT) and endothelium (eNOS) were protected. Thus, the integrity of venous occlusive mechanism was preserved and the erectile function was improved (ICP/MAP). The improved erectile function was also a favorable factor for penile size preservation. Additionally, arterial blood may not only provide oxygen to the corporal tissues, it may also carry other nutrients such as certain growth factors to the tissues which may also contribute to penile recovering. This concept needs to be confirmed in future studies. The possible mechanisms for VED therapy after RP are summarized in Figure 2.
Conclusions
There are clinical and basic scientific evidences showing that VED therapy improves erectile function and preserves penile size after cavernous nerve injury. The beneficial effect of VED therapy may be related to anti-hypoxic, anti-apoptotic and anti-fibrotic mechanisms. However, well designed clinical studies with long-term follow up are not available at this time. Multi-center, randomized studies to compare the effectiveness of VED vs. PDE5i vs. penile injection or transurethral use of vasodilators in penile rehabilitation after RP should be considered.
Acknowledgements
The authors would like to thank Ms. Dorothy Stradinger for her editorial assistance.
Footnote
Conflicts of Interest: Run Wang, MD, FACS, Investigator: The American Medical System, Inc., Coloplast Inc., Vivus, Inc., Timm Medical, Inc., and UroMatrix Medical Systems; Consultant: Coloplast Inc., Timm Medical, Inc., MenMD, Inc. The other author has no conflicts of interest to declare.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10-29. [PubMed]
- Novara G, Ficarra V, Rosen RC, et al. Systematic review and meta-analysis of perioperative outcomes and complications after robot-assisted radical prostatectomy. Eur Urol 2012;62:431-52. [PubMed]
- Burnett AL, Aus G, Canby-Hagino ED, et al. Erectile function outcome reporting after clinically localized prostate cancer treatment. J Urol 2007;178:597-601. [PubMed]
- Yu Ko WF, Degner LF, Hack TF, et al. Penile length shortening after radical prostatectomy: men’s responses. Eur J Oncol Nurs 2010;14:160-5. [PubMed]
- Vasconcelos JS, Figueiredo RT, Nascimento FL, et al. The Natural History of Penile Length After Radical Prostatectomy: A Long-term Prospective Study. Urology 2012;80:1293-6. [PubMed]
- Fraiman MC, Lepor H, McCullough AR. Changes in Penile Morphometrics in Men with Erectile Dysfunction after Nerve-Sparing Radical Retropubic Prostatectomy. Mol Urol 1999;3:109-115. [PubMed]
- Munding MD, Wessells HB, Dalkin BL. Pilot study of changes in stretched penile length 3 months after radical retropubic prostatectomy. Urology 2001;58:567-9. [PubMed]
- Savoie M, Kim SS, Soloway MS. A prospective study measuring penile length in men treated with radical prostatectomy for prostate cancer. J Urol 2003;169:1462-4. [PubMed]
- Wang R. Penile rehabilitation after radical prostatectomy: where do we stand and where are we going? J Sex Med 2007;4:1085-97. [PubMed]
- Mulhall JP, Morgentaler A. Penile rehabilitation should become the norm for radical prostatectomy patients. J Sex Med 2007;4:538-43. [PubMed]
- Teloken P, Mesquita G, Montorsi F, et al. Post-radical prostatectomy pharmacological penile rehabilitation: practice patterns among the international society for sexual medicine practitioners. J Sex Med 2009;6:2032-8. [PubMed]
- Tal R, Teloken P, Mulhall JP. Erectile function rehabilitation after radical prostatectomy: practice patterns among AUA members. J Sex Med 2011;8:2370-6. [PubMed]
- Yuan J, Westney OL, Wang R. Design and application of a new rat-specific vacuum erectile device for penile rehabilitation research. J Sex Med 2009;6:3247-53. [PubMed]
- Yuan J, Hoang AN, Romero CA, et al. Vacuum therapy in erectile dysfunction--science and clinical evidence. Int J Impot Res 2010;22:211-9. [PubMed]
- Hinh P, Wang R. Overview of contemporary penile rehabilitation therapies. Adv Urol 2008.481218. [PubMed]
- Köhler TS, Pedro R, Hendlin K, et al. A pilot study on the early use of the vacuum erection device after radical retropubic prostatectomy. BJU Int 2007;100:858-62. [PubMed]
- Burnett AL. Rationale for cavernous nerve restorative therapy to preserve erectile function after radical prostatectomy. Urology 2003;61:491-7. [PubMed]
- Dean RC, Lue TF. Neuroregenerative strategies after radical prostatectomy. Rev Urol 2005;7:S26-32. [PubMed]
- Walsh PC. Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. J Urol 2000;164:242. [PubMed]
- Moreland RB, Traish A, McMillin MA, et al. PGE1 suppresses the induction of collagen synthesis by transforming growth factor-beta 1 in human corpus cavernosum smooth muscle. J Urol 1995;153:826-34. [PubMed]
- Leungwattanakij S, Bivalacqua TJ, Usta MF, et al. Cavernous neurotomy causes hypoxia and fibrosis in rat corpus cavernosum. J Androl 2003;24:239-45. [PubMed]
- Granchi S, Vannelli GB, Vignozzi L, et al. Expression and regulation of endothelin-1 and its receptors in human penile smooth muscle cells. Mol Hum Reprod 2002;8:1053-64. [PubMed]
- Moreland RB, Gupta S, Goldstein I, et al. Cyclic AMP modulates TGF-beta 1-induced fibrillar collagen synthesis in cultured human corpus cavernosum smooth muscle cells. Int J Impot Res 1998;10:159-63. [PubMed]
- Gontero P, Kirby R. Proerectile pharmacological prophylaxis following nerve-sparing radical prostatectomy (NSRP). Prostate Cancer Prostatic Dis 2004;7:223-6. [PubMed]
- Mulhall JP, Graydon RJ. The hemodynamics of erectile dysfunction following nerve-sparing radical retropubic prostatectomy. Int J Impot Res 1996;8:91-4. [PubMed]
- Mulhall JP, Slovick R, Hotaling J, et al. Erectile dysfunction after radical prostatectomy: hemodynamic profiles and their correlation with the recovery of erectile function. J Urol 2002;167:1371-5. [PubMed]
- User HM, Hairston JH, Zelner DJ, et al. Penile weight and cell subtype specific changes in a post-radical prostatectomy model of erectile dysfunction. J Urol 2003;169:1175-9. [PubMed]
- Podlasek CA, Meroz CL, Tang Y, et al. Regulation of cavernous nerve injury-induced apoptosis by sonic hedgehog. Biol Reprod 2007;76:19-28. [PubMed]
- Mulhall JP. Penile length changes after radical prostatectomy. BJU Int 2005;96:472-4. [PubMed]
- User HM, Hairston JH, Zelner DJ, et al. Penile weight and cell subtype specific changes in a post-radical prostatectomy model of erectile dysfunction. J Urol 2003;169:1175-9. [PubMed]
- Zippe CD, Raina R, Thukral M, et al. Management of erectile dysfunction following radical prostatectomy. Curr Urol Rep 2001;2:495-503. [PubMed]
- Zippe CD, Pahlajani G. Vacuum erection devices to treat erectile dysfunction and early penile rehabilitation following radical prostatectomy. Curr Urol Rep 2008;9:506-13. [PubMed]
- Turner LA, Althof SE, Levine SB, et al. External vacuum devices in the treatment of erectile dysfunction: a one-year study of sexual and psychosocial impact. J Sex Marital Ther 1991;17:81-93. [PubMed]
- Cookson MS, Nadig PW. Long-term results with vacuum constriction device. J Urol 1993;149:290-4. [PubMed]
- Raina R, Agarwal A, Ausmundson S, et al. Early use of vacuum constriction device following radical prostatectomy facilitates early sexual activity and potentially earlier return of erectile function. Int J Impot Res 2006;18:77-81. [PubMed]
- Dalkin BL, Christopher BA. Preservation of penile length after radical prostatectomy: early intervention with a vacuum erection device. Int J Impot Res 2007;19:501-4. [PubMed]
- Yuan J, Lin H, Li P, et al. Molecular mechanisms of vacuum therapy in penile rehabilitation: a novel animal study. Eur Urol 2010;58:773-80. [PubMed]
- Bosshardt RJ, Farwerk R, Sikora R, et al. Objective measurement of the effectiveness, therapeutic success and dynamic mechanisms of the vacuum device. Br J Urol 1995;75:786-91. [PubMed]


