Determinants of doctors’ decisions to inquire about sexual dysfunction in Malaysian primary care settings
Introduction
Erectile dysfunction (ED) and premature ejaculation are common male sexual dysfunctions but under-reported globally (1-5). In a review published in 2002 and a multinational study in 2004, the prevalence of ED ranged from 2% for men younger than 40 years to 71% for men older than 70 (4,5) whereas for Malaysian men older than 40 years old, the prevalence of moderate to severe ED, which was defined as an International Index of Erectile Function-5 (IIEF-5) score of less than 17, ranged from 37.3% to 53.6% (1-3). In primary care settings in Malaysia, the estimated prevalence of ED was 64.5% (6). Unfortunately, although prevalent, ED is often under-reported by patients (6,7). A Malaysian community survey involving 1,046 men aged 40 and above in an urban area found that only 21% of men self-reported ED, despite 65.5% of them having been noted to have some form of ED (8). Premature ejaculation is another common sexual dysfunction in men that has a significant impact on men’s health. In a few reviews and multinational studies between 2005 and 2010, 20% to 30% of men across all age groups and countries were reported to suffer from premature ejaculation (9-11). The prevalence was noted to be higher (66%) in primary care settings (11). Also, even with such high prevalence, very few patients (an estimated 9% of men with premature ejaculation) seek help (12).
Assessing sexual dysfunction is important because of its clinical significance. ED acts as the sentinel marker for cardiovascular disease in men age >40 years old (2,13). It is associated with cardiovascular risk factors (2,14-16) and predicts future events of cardiovascular related diseases such as diabetes, hypertension, hyperlipidaemia and angina (17). Besides, men who suffer from sexual dysfunctions have significant psychosocial morbidities and relationship problems (12,18-21). More importantly, effective treatment for ED and premature ejaculation is available. Therefore, assessment of sexual dysfunction is warranted especially if presence of risk factors such as older age groups and cardiovascular risk factors. Primary care consultation offers such opportunity (22).
However, sexual dysfunction is often not discussed in consultations with male patients (23-25). Primary care doctors seldom actively seek out sexual history in their consultations with men (23,26-29), unless there is a pressing need to address the issue (30) such as at the initiative of the male patients (28) during family planning sessions, in encounters with sexually transmitted disease (23,31), chronic illnesses and smoking (23,24,32). It is less commonly undertaken as a routine assessment (24,30,32) despite awareness of its importance (23,30). An earlier qualitative study has noted that primary care doctors’ perception of men’s receptivity to health check-ups is one of the determinants in explaining whether doctors would initiate health check-up discussions with their male patients (25). It also offers a conceptual framework explaining the decision making process of primary care doctors to engage male patients in health check-ups (25). In the context of sexual dysfunction, perceptions of medical importance of assessing sexual dysfunction, external factors such as tight clinic schedule and personal competency in managing sexual dysfunction are also postulated to determine the doctors’ decision making. However, because of the qualitative approach, we are unable to determine the extent of the doctors’ perception of men’s receptivity to discuss sexual dysfunction, nor the relative importance among the determinants in the process of doctors’ decision making. The aim of this study is to determine the relative importance of doctors’ perceptions of men’s receptivity and other determinants on male sexual health inquiry by primary care doctors. This study was part of the a larger study to quantify the impact of the determinants on primary care doctors’ decision to engage in men’s health check-ups in five areas of men’s health concern at outpatient settings. The five areas are cardiovascular risk assessment, asking about sexual dysfunction, psychosocial health assessment, asking about smoking and colon cancer screening. This paper examines specifically at male sexual dysfunction.
Methods
Study design and sampling
This was a cross sectional study among randomly selected primary care doctors from two selected states (i.e., Kelantan and Selangor—including Kuala Lumpur) in Malaysia. In Malaysia, primary care service is provided by private (patient funded) and public (government funded) sectors. On an average, each private clinic has one residential doctor compared to three to five doctors per clinic in public sector.
Conceptual framework and survey instruments
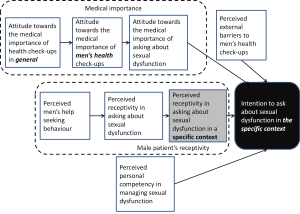
The conceptual framework was developed based on the proposed model from the qualitative study (Figure 1) (9). Four main categories of determinants were constructed with a total of twelve determinants. The categories of medical importance comprised three constructs of doctors’ attitudes towards the issues of health check-ups and sexual dysfunction. The categories of perception of male patient’s receptivity also comprised three constructs of receptivity to heath check-ups (Figure 1). According to the proposed model (9), the perceived receptivity of male patients to the assessment of sexual dysfunction was closely related to the three different contexts of consultations—minor complaints visits, follow-up visits and health checks visits. The items assessing perceived male patients’ receptivity in a specific context asked for doctors’ agreement whether a middle age man would “feel offended”, “accept” or “think of me as being weird” if they raised the issue of sexual dysfunction during: (I) acute minor complaint; (II) follow-up visits; (III) wellness check-ups. The remaining determinants were the five external barriers to health check-ups (time constraint, lack of clinic system supporting health check-up, lack of privacy in the clinic, lack of referral network and cost constraint to men) and the final one determinant—the perceived personal competence in managing sexual dysfunction (Figure 1). The outcome variable was doctor’s intention in asking about sexual dysfunction in a middle age man in the respective three contexts of consultation. It was postulated the likeliness of asking about sexual dysfunction would differ between different contexts of consultation—more likely in health checks visits than minor complaints visits (9).
Questionnaires were developed to measure each of the concepts in the framework. Each determinant (explanatory variable) was measured with 2-5 items. The response to the items was also measured on the Likert scale of 1 to 5 denoting “strongly disagree” to “strongly agree”. The outcome variable was assessed with a single question asking how likely were the doctor to ask about patient’s sexual dysfunction in the respective contexts. The response was measured on Likert scale ranging from 1 to 5 denoting strongly unlikely to strongly likely. The initial set of questionnaires, comprising 66 items was developed based on the same model used in the conceptual framework and underwent validation for face validity, structural validity and internal consistency. five experts (one senior consultant primary care doctor, three local primary care doctors and one clinical psychologist) participated in the face validation whereas 91 primary care doctors, who were not the participants in this study, participated in structural validation and internal consistency testing. The final set of questionnaires used for field study comprised 49 items. The KMO statistics, factor loadings and Cronbach α for each of the concepts ranged from 0.500-0.835, 0.582-0.911 and 0.545-0.868 respectively. The questionnaires demonstrated acceptable construct validity and internal consistency. Hence, the aggregate score were used in data analysis.
Sampling and sample size
The participants were randomly selected from a registry of primary care clinics. Although the unit of analysis was primary care doctors (PCDs), the listing of PCDs was unavailable. Instead, there were registries for primary care clinics. Hence, the sampling unit was the primary care clinics and all the doctors from the selected clinics were invited to participate. The sample size was calculated with the Epi Info StatCalc 2000® program using an estimated 50% response rate with a lowest acceptable rate of 40%. The sampling was stratified to private and public doctors. Because of different population size of public and private sectors, the estimated number of private doctors needed was 91 and 82 for public clinics. A further 50% was added to account for non-responders, which resulted in 182 private doctors and 164 doctors in public clinics, with a total of 346 doctors, to be recruited. With the assumption of each private clinic would have a resident doctor, 182 private clinics were selected from the 2007 (the latest version) Malaysian Medical and Health Directory using Window Excel® random number function. Whereas, assuming each public clinic had four doctors, 38 public clinics were selected from the Health Facility Registry of the Ministry of Health Malaysia 2007. The resident doctors of each selected clinics were approached by telephone and asked to have an appointment to explain about the survey. To be eligible to participate, they must be practicing primary care doctors who see general outpatients. They were visited and then given the questionnaire if consenting to participate. A book about men’s health was given to each respondent as a token of appreciation after the returning of completed questionnaire. The questionnaire was returned by post or was collected on the same visit.
Data analysis
The data were entered and analysed with Statistical Package for Social Science Study (SPSS for Window, release 16.0.1. 2007. Chicago: SPSS Inc). Missing data were not replaced. Descriptive statistics were used to illustrate the characteristics of the respondents. The mean scores were used to describe the primary care doctors’ views on various concepts measured. To determine the independent strength of the association between each of the explanatory variables and the outcome variable, simultaneous ordinal least square model was used because the outcome variable was measured in ordinal categorical scale. The factor scores of all the concepts in the determinants were used in the regression analysis because they would yield better validity compared to mean scores (33). Appropriate link functions (Negative log-log, Logit or Complementary log-log) for the regression model was chosen depending on the frequency distribution of outcome variable. Three models were constructed to include all determinants consistent with three contexts of consultation. The fitness of the model was tested using χ2 test of -2log-likelihood values between model with only intercept and model with all explanatory variables and Pearson and Deviance goodness-of-fit measures. The relevance of the model was assessed using Nagelkerke’s R2. The significant level was set at P<0.05. Tests of parallelism in all three models showed a non-significant difference (P>0.05) between null hypothesis (which states that the regression slopes are parallel) and the models (which makes no assumption of parallelism), confirming the valid use of ordinal regression analysis.
Results
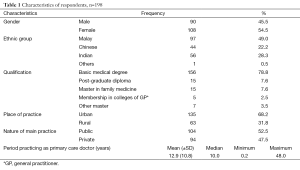
A total of 224 clinics were sampled from the registries instead of the planned 220. 185 private and 38 public clinics were visited. 280 doctors were invited because some clinics had more than one resident doctor especially in the public clinics. However, the overall response rate was 70.4% (n=198), higher than the needed 173. The majority of participants were Malay, had basic medical degrees and were in urban practices (Table 1). There were slightly less male participants and fewer participants from the private sector. The period practicing as PCDs among the participants varied widely (Table 1); they skewed to shorter periods. The majority of doctors had ≤10.0 years of experience.
Full table
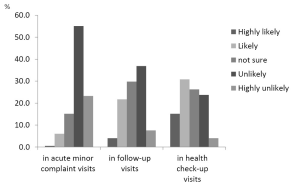
Although majority of doctors were very unlikely or unlikely to ask about sexual dysfunction in their consultation especially during acute minor complaint visits, more doctors were likely or very likely to do so in health check-up visits (Figure 2). There was substantial percentage (26.3-29.8%) of doctors unsure about their intention to ask about sexual dysfunction in follow-up or health check-up visits (Figure 2). Only 25.8% and 46% of doctors intended to ask about sexual dysfunction in the follow-up and health check-up visits of a middle age man respectively.
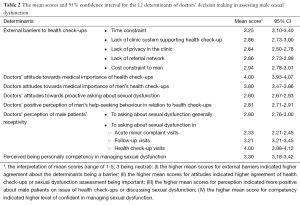
Among five external barriers assessed, time constraint was described as the most important barriers in assessing male sexual dysfunction (Table 2). The primary care doctors were positive towards the importance of general health check-ups and men’s health check-ups for male patients, with a mean score of 3.8 and 4.0 respectively. However, they were less certain about the medical importance of proactive asking about sexual dysfunction, with a mean score of 2.8. Generally, primary care doctors had a perception of male patients being not keen in health check-ups (with a mean score of 2.8) and did not think male patients were receptive if they were asked about sexual dysfunction. However, during consultation for follow-up visits and health check-ups, male patients could be receptive to discuss about sexual dysfunction, with mean scores of 3.2-4.0. The primary care doctors were rather confident in managing sexual dysfunction, with a self-competency score of 3.30.
Full table
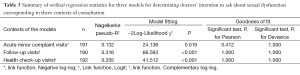
All three models, corresponding to three contexts of consultation, significantly explained 13.2% to 31.6% of the variability of doctors’ intention to ask about sexual dysfunction (Table 3). All three models have significant model fitting statistics of –2log-likelihood χ2 (Table 3). The non-significant of goodness-of-fit statistics indicated the tested models fitted well with the observed data. However, the model best explained doctor’s intention to ask about sexual dysfunction in the context of follow-up visits and least well in acute minor complaint visits (Table 3).
Full table
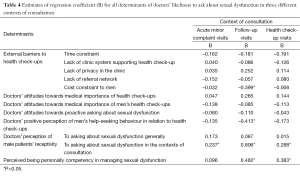
The relative importance of each determinant from the others was ascertained by comparing the coefficient estimates of regression, B, of the variable from the ordinal regression models. Doctor’s perception of receptivity was the most significant determinant in explaining doctor’s intention to ask about sexual dysfunction (Table 4)—the determinant with the most frequent highest B compared to the other determinants. Doctor’s perception of higher degree of men’s receptivity to asking about sexual dysfunction increased the likeliness of doctors in asking about sexual dysfunction in all three contexts (B=0.237 in acute minor complaint visits, B=0.806 in follow-up visits, B=0.288 in health check-up visits), and it was the most important determinant in acute minor complaint and follow-up visits, with the highest B (Table 4). The perceived receptivity was specific to the context of consultation. Perceived higher degree of personal competence in assessing sexual dysfunction was also a significant determinant in the doctors’ intention to enquire about sexual dysfunction in the follow-up visits and health checks visits, but not in acute minor complaint visits. Cost constraint and perceived help seeking behaviour were other two important determinants in the doctor’s intention only in the follow-up visits, not with the other two contexts of consultation (Table 4).
Full table
Discussion
Despite its significant impact on health, sexual dysfunction, and ED in particular, is considered a sensitive subject and is seldom talked about in primary care outpatient encounters in Malaysia (34). In this study, a majority of the doctors were also unlikely to ask about sexual dysfunction unless in a specific visit for health check-ups. Even then, a quarter of doctors were unsure whether to ask about sexual dysfunction. The explanation for doctor’s intention to ask about sexual dysfunction was explored by examining the conceptual models constructed and the significant determinants in the model in predicting the doctors’ intention. We found the models significantly explained 13% to 32% of the variance in their intention to ask about sexual dysfunction. We also found the most significant determinant was the doctor’s perception of male patient’s receptivity to discuss sexual dysfunction. Not unexpected, perceived personal competency in managing sexual dysfunction also significantly predicted the doctor’s intention. However, it was interesting to note that the attitudes towards the medical importance of sexual dysfunction did not significantly predict the doctor’s intention.
The doctors in this study perceived male patients as being unreceptive to asking about sexual dysfunction, especially in the context of acute minor complaint visits. This is similar to many other studies on the barriers to asking about sexual dysfunction in primary care settings (23,24,28,34,35). Primary care doctors presumed that men would feel uncomfortable talking about sexual health if the issues were not initiated by them, thereby keeping the doctors from proactively talking about it (23). They preferred that patients raise the issue of sexual health (24,28), worrying that their male patients would be suspicious of their intentions if sexual health issues were raised without apparent reason (35). Similar findings on this issue relating to ED have also been revealed in a qualitative study among 28 primary care doctors in Malaysia (34). In that study, the doctors regarded ED as a non-serious illness and one that was taboo. They were more comfortable if male patients raised the topic for discussion, seeing themselves as mere facilitators and being concerned at being stigmatized as drug pushers if active screening for ED was undertaken (34). However, these are descriptive studies and the impact of these doctors’ opinions on their practice behaviour has not been confirmed. On the other hand, the current study, by using regression analysis, provides stronger evidence that the doctors’ negative perceptions of male patients’ receptivity, which included perceived patient comfort in discussing sexual dysfunction, is negatively affecting their practice behavior—i.e., they are less likely to raise the issue of sexual dysfunction.
Similarly, while doctors’ personal competency in addressing ED is also described in other studies as a barrier to initiating discussion about ED (26,31,32,35-37), this study demonstrates that a perceived higher degree of personal competency is positively correlated with doctors’ intention to ask about sexual dysfunction in health check-up visits. It is interesting to note that perceived personal competency is not the most significant barrier in acute minor complaint and follow-up visits. Instead, perceived male patients’ receptivity is the main barrier as described above. Therefore, this study has further stratified the important determinants specific to the contexts of consultation which other studies have not shown.
In other studies, the barriers identified in addressing sexual health in clinic settings include lack of time (24,26,31,37), resources constraints and lack of confidentiality during consultation (31,37). These barriers are also described in this study in Table 2 particularly time constraint, but the regression analysis shows the only significant determinant was the negative impact of cost constraints on doctors’ intention to ask about sexual dysfunction in follow-up visits. Therefore, the significance of external factors as barriers may be overestimated. Nevertheless, the findings may not represent the views of individual doctors, but rather the average views of all doctors. To an individual doctor, all the external barriers described may appear to significantly impact his or her practice.
However, doctors’ views of male patients may not reflect male patients’ opinions. In fact, doctors’ perceptions can be inaccurate, as in the case of doctors’ perceptions of men’s help-seeking behaviour. On the contrary, most male patients would like their doctors to raise the issue (23,38-41) and preferred that their family doctors be the source of help (42). They see the proactive role of GPs in asking about sexual history as a license to talk about sexual health (39). Hence, doctors’ perceptions of male patients’ non-receptivity and discomfort in discussing sexual dysfunction may be a myth.
Managing male sexual dysfunction in primary care settings is challenging because it is a sensitive issue and a taboo subject for male patients. Although the issue of managing sexual dysfunction from the doctors’ perspective has drawn considerable attention in an attempt to improve diagnostic rates and service delivery, most of the studies tend to be descriptive. This study has managed to demonstrate the impact of perceived male patients’ receptivity and personal competency on doctors’ intentions to ask about sexual dysfunction in primary care clinic settings. This study has also managed to identify the relative importance of these determinants in different contexts of consultation. As a whole, this study proves the relevance of the conceptual framework in explaining the doctors’ intention in asking about sexual dysfunction in male patients.
This study demonstrated the models being able to explain only 13% to 32% of the variance in the doctor’s intention to ask about sexual dysfunction. Although a large proportion of the variances are unaccounted for, the model is considered to have good explanatory property in psychological research (43). The large proportion of unaccounted variances could be the result of a high variability in individual doctor’s emphasis on a determinant in the model. One doctor may emphasise medical importance, another external barriers in his/her decision to engage male patients in asking about sexual dysfunction. Because of quantitative nature of this study, which represents a normative pattern of phenomenon of interest, only an average picture can be shown. An individual doctor’s decision-making process does not necessarily conform to the normative pattern of the decision-making process.
On the issue of sampling, the stratified random sampling and good response rate (70%) enhance the external validity of this study. Although there is no agreed threshold for a good response rate, 70% can be considered excellent since random surveys among primary care doctors often have less than a 50% response rate. The sample size calculated did not account for clustering effect, where all doctors in the clinic sampled were invited to participate. Given the clinics were the sampling unit rather than the doctors and the doctors in a same clinic may share similar characteristics, the standard errors may be inflated hence affect the statistical significance of the result. Sample size could have been larger to minimise type I error in this study. This might be an issue for public clinics because private clinics would usually have only one resident doctor as opposed to 3-5 doctors in public clinics. However, the clustering effect is likely small because in this survey, only one private clinic has two participating doctors and the mean number of participating doctors in public clinic was 2.75. Therefore, the results of this study would likely stay similar even if clustering effect is considered in sample size calculation.
Conclusions
Whilst sexual health inquiry should be initiated in an appropriate context, ‘perceived receptivity’ to sexual health inquiry significantly affected doctors’ intention in initiating sexual health inquiry to their male patients. Contrary to the doctors’ perceptions, male patients’ appear to be receptive to questions about sexual dysfunction. Therefore, the unfounded perception of men being unreceptive to questioning about sexual dysfunction is an area that needs attention in order to improve the management of sexual dysfunction. In addition, doctors’ competency in managing sexual dysfunction, ED in particular, should be a focus of attention. Malaysian men’s health may be substantially improved by strategies that assist doctors to identify patient’s ‘receptivity’. This will help doctors making better decision to initiate discussing sexual dysfunction.
Acknowledgements
We would like to thank University of Malaya for the ethics approval and funding the study. We also wish to thank the Human Research Ethics Committee for approving the study and the Director General of Health of the Ministry of Health for granting the permission to conduct and support to publish. We greatly appreciate the contribution of all participating primary care doctors in providing valuable data to the study.
Funding: This work was supported by Short-Term-Research-Grant from the University of Malaya [FS241/2008C]. The funding institution has no role at all in the design, conduct and analysis of the study, and the writing and submission of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical approval: The study was approved by the ethics committees from the University of Malaya (679.28), the Ministry of Health Malaysia (NMRR-09-710-4499), and the University of Sydney (11-2009/12262).
References
- Quek KF, Sallam AA, Ng CH, et al. Prevalence of sexual problems and its association with social, psychological and physical factors among men in a Malaysian population: a cross-sectional study. J Sex Med 2008;5:70-6. [PubMed]
- Khoo EM, Tan HM, Low WY. Erectile dysfunction and comorbidities in aging men: an urban cross-sectional study in Malaysia. J Sex Med 2008;5:2925-34. [PubMed]
- Mariappan P, Chong WL. Prevalence and correlations of lower urinary tract symptoms, erectile dysfunction and incontinence in men from a multiethnic Asian population: Results of a regional population-based survey and comparison with industrialized nations. BJU Int 2006;98:1264-8. [PubMed]
- Prins J, Blanker MH, Bohnen AM, et al. Prevalence of erectile dysfunction: a systematic review of population-based studies. Int J Impot Res 2002;14:422-32. [PubMed]
- Rosen RC, Fisher WA, Eardley I, et al. The multinational Men’s Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin 2004;20:607-17. [PubMed]
- Asnida AAR, Nabilla AS. Erectile dysfunction in primary care setting. Malaysian Family Physician 2009;4:28.
- Shabsigh R, Kaufman J, Magee M, et al. Lack of awareness of erectile dysfunction in many men with risk factors for erectile dysfunction. BMC Urol 2010;10:18. [PubMed]
- Ng CJ, Tan HM, Khoo EM, et al. Under-detection and under treatment of common men’s health problems. Asian J Androl 2007;9:418.
- Porst H, Montorsi F, Rosen RC, et al. The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: prevalence, comorbidities, and professional help-seeking. Eur Urol 2007;51:816-23. [PubMed]
- Montorsi F. Prevalence of premature ejaculation: a global and regional perspective. J Sex Med 2005;2 Suppl 2:96-102. [PubMed]
- Jannini EA, Lenzi A. Epidemiology of premature ejaculation. Curr Opin Urol 2005;15:399-403. [PubMed]
- Althof SE, Abdo CH, Dean J, et al. International Society for Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med 2010;7:2947-69. [PubMed]
- Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med 2007;120:151-7. [PubMed]
- Ahn TY, Park JK, Lee SW, et al. Prevalence and risk factors for erectile dysfunction in Korean men: results of an epidemiological study. J Sex Med 2007;4:1269-76. [PubMed]
- Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med 2007;120:151-7. [PubMed]
- Grover SA, Lowensteyn I, Kaouache M, et al. The prevalence of erectile dysfunction in the primary care setting: importance of risk factors for diabetes and vascular disease. Arch Intern Med 2006;166:213-9. [PubMed]
- Shabsigh R, Shah M, Sand M. Erectile dysfunction and men’s health: developing a comorbidity risk calculator. J Sex Med 2008;5:1237-43. [PubMed]
- Low WY, Tong SF, Tan HM. Erectile dysfunction, premature ejaculation and hypogonadism and men’s quality of life: an Asian perspective. J Mens health 2008;5:282-8.
- Wagner G, Fugl-Meyer KS, Fugl-Meyer AR. Impact of erectile dysfunction on quality of life: patient and partner perspectives. Int J Impot Res 2000;12:S144-6. [PubMed]
- Litwin MS, Nied RJ, Dhanani N. Health-related quality of life in men with erectile dysfunction. J Gen Intern Med 1998;13:159-66. [PubMed]
- Althof SE. Quality of life and erectile dysfunction. Urology 2002;59:803-10. [PubMed]
- Green LA, Fryer GE Jr, Yawn BP, et al. The ecology of medical care revisited. N Engl J Med 2001;344:2021-5. [PubMed]
- Aschka C, Himmel W, Ittner E, et al. Sexual problems of male patients in family practice. J Fam Pract 2001;50:773-8. [PubMed]
- Perttula E. Physician attitudes and behaviour regarding erectile dysfunction in at-risk patients from a rural community. Postgrad Med J 1999;75:83-5. [PubMed]
- Tong SF, Low WY, Ismail SB, et al. Physician’s intention to initiate health check-up discussions with men: a qualitative study. Fam Pract 2011;28:307-16. [PubMed]
- Broekman CP, van der Werff ten Bosch JJ, Slob AK. An investigation into the management of patients with erection problems in general practice. Int J Impot Res 1994;6:67-72. [PubMed]
- Platano G, Margraf J, Alder J, et al. Frequency and focus of sexual history taking in male patients--a pilot study conducted among Swiss general practitioners and urologists. J Sex Med 2008;5:47-59. [PubMed]
- De Berardis G, Pellegrini F, Franciosi M, et al. Management of erectile dysfunction in general practice. J Sex Med 2009;6:1127-34. [PubMed]
- Andrews CN, Piterman L. Sex and the older man--GP perceptions and management. Aust Fam Physician 2007;36:867-9. [PubMed]
- Wimberly YH, Hogben M, Moore-Ruffin J, et al. Sexual history-taking among primary care physicians. J Natl Med Assoc 2006;98:1924-9. [PubMed]
- Temple-Smith MJ, Mulvey G, Keogh L. Attitudes to taking a sexual history in general practice in Victoria, Australia. Sex Transm Infect 1999;75:41-4. [PubMed]
- Tsimtsiou Z, Hatzimouratidis K, Nakopoulou E, et al. Predictors of physicians’ involvement in addressing sexual health issues. J Sex Med 2006;3:583-8. [PubMed]
- DiStefano C, Zhu M, Mîndrilă D. Understanding and Using Factor Scores: Considerations for the Applied Researcher. Practical Assessment, Research & Evaluation 2009;14:2.
- Ng CJ, Low WY, Tan NC, et al. The role of general practitioners in the management of erectile dysfunction-a qualitative study. Int J Impot Res 2004;16:60-3. [PubMed]
- Poljski C, Tasker C, Andrews C, et al. GP attitudes to male reproductive and sexual health education and promotion. A qualitative study. Aust Fam Physician 2003;32:462-5. [PubMed]
- Gott M, Galena E, Hinchliff S, et al. “Opening a can of worms”: GP and practice nurse barriers to talking about sexual health in primary care. Fam Pract 2004;21:528-36. [PubMed]
- Low WY, Ng CJ, Tan NC, et al. Management of erectile dysfunction: barriers faced by general practitioners. Asian J Androl 2004;6:99-104. [PubMed]
- Low WY, Tan HM, Tong SF, et al. eds. About Men’s Health: Views from Mars and Venus. 2nd ed. Kuala Lumpur: MSASAM, 2010.
- Read S, King M, Watson J. Sexual dysfunction in primary medical care: prevalence, characteristics and detection by the general practitioner. J Public Health Med 1997;19:387-91. [PubMed]
- Nazareth I, Boynton P, King M. Problems with sexual function in people attending London general practitioners: cross sectional study. BMJ 2003;327:423. [PubMed]
- Metz ME, Seifert MH Jr. Men’s expectations of physicians in sexual health concerns. J Sex Marital Ther 1990;16:79-88. [PubMed]
- Dunn KM, Croft PR, Hackett GI. Sexual problems: a study of the prevalence and need for health care in the general population. Fam Pract 1998;15:519-24. [PubMed]
- Cohen J, Cohen P, West SG, et al. eds. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ; London: Lawrence Erlbaum Associates, 2003.