The argument for palliative care in prostate cancer
Palliative care uses a team approach to improve the quality of life of patients and families faced with long-term and progressive illnesses through prevention and relief of suffering with symptom management. Palliative care focuses on three main realms to achieve these goals: morbidities associated with the disease, morbidities associated with the treatment, and quality of life of the patient. Oncology guidelines suggest initiating palliative care “early in the course of illness in conjunction with other therapies that are intended to prolong life, including chemotherapy and radiation” (1). Possibly due to the association with end of life care, palliative care is under-utilized for prostate cancer despite evidence showing benefit in several patient populations.
Prostate cancer is particularly amenable to palliative symptom management because of its long disease course and, often, non-lethal progressive nature. It is the most common cancer diagnosis in American males and there are expected to be almost 240,000 American men diagnosed with prostate cancer in 2013 (2). Of those staged at diagnosis, 80% will have localized disease, 12% will have regional disease, and 4% will have metastatic disease (3). Disease specific morbidity worsens as prostate cancer progresses and can include bony metastases, spinal cord compression, lymphedema, urinary obstruction, fatigue, anemia, and significant psychological effects including depression, anxiety, poor coping ability, altered view of self and future, lack of empowerment, and disrupted partner intimacy (4). The treatments for prostate cancer vary by stage but all may be associated with morbidity. Localized treatment with surgery and/or radiation is associated with side effects including pain, erectile dysfunction, incontinence, bowel dysfunction, fatigue, dysuria, gross hematuria, and urethral stricture development (5). Men who develop biochemical recurrence after localized therapy and men who are diagnosed with regional or metastatic disease may be treated with androgen deprivation which can cause side effects including nausea, vomiting, diarrhea, hot flashes, loss of libido, gynecomastia, insomnia, gastric ulceration, immune suppression, psychiatric effects, myalgias, weight gain, osteoporosis, and lower urinary tract symptoms (6). A number of novel therapies including chemotherapies, targeted-hormonal therapies, and immunotherapies have been developed for castrate-resistant prostate cancer in recent years that can prolong survival on average two to four months, however they may be associated with a number of severe side-effects (Table 1). In light of the significant disease and treatment morbidities associated with prostate cancer it is not surprising that Torvinen et al. found markedly worsened quality of life across the three realms of palliative care as prostate cancer progressed from localized to metastatic disease (7).
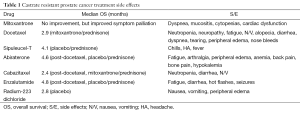
Full table
The literature overwhelmingly supports the utilization of palliative care in both long-term illness and various forms of cancer. Multiple randomized trials have demonstrated significantly improved quality of life, decreased symptom intensity, improved patient satisfaction, longer hospice stays, lower health care costs, and less aggressive end-of-life care (8,9). One of the most widely discussed and intriguing trials by Temel et al. showed significantly longer median survival (11.6 vs. 8.9 months, P<0.02) after implementation of palliative care for patients with non-small-cell lung cancer (10). The limited data examining palliative care specifically in prostate cancer also supports its use. A retrospective review at MD Anderson found that the most common symptoms reported by men with advanced prostate cancer included fatigue, drowsiness and pain. After palliative care intervention patients had statistically significant improvement in those symptoms as well as sleep, well-being, anxiety and depression (11). Rabow et al. found that men with prostate cancer undergoing palliative care in addition to their oncologic or surgical management had significant improvements in fatigue (P=0.02), anxiety (P<0.01), depression (P<0.01), quality of life (P<0.01) and spiritual well-being (P<0.01) (12).
However, referrals to palliative care typically occur late in the disease process because of its inappropriate association with end-of-life care and failure to recognize that symptom management can be utilized throughout the course of a disease. Dalal et al. found that one barrier to care was the name “palliative care” itself. After changing their group’s name from “palliative care” to “supportive care” they received an increase in consultations and shorter duration from the time of diagnosis to consultation (13). Similar to the change in terminology from “watchful waiting” to “active surveillance” indicating use in different patient populations and treatment interventions, perhaps palliative care would benefit from a name change to broaden its recognition and allow patients with non-life-threatening disease to benefit from its incorporation into routine care.
Palliative care used in conjunction with prostate cancer treatment can significantly improve patient quality of life however it is rarely implemented early in the disease process. With nearly 38,000 men expected to be diagnosed with regional or metastatic prostate cancer this year and an expected 30,000 deaths from prostate cancer in 2013 it is imperative that we begin to follow the guidelines and initiate symptom-modifying palliative care along with disease-modifying therapies.
Acknowledgements
The authors would like to acknowledge Michael Rabow MD for his guidance in this topic and his current work in palliative care at UCSF.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- World Health Organization website. WHO Definition of Palliative Care. Available online: , accessed 2013 Aug 19.http://www.who.int/cancer/palliative/definition/en/
- American Cancer Society website. Cancer Facts & Figures 2013. Available online: , accessed 2013 Aug 19.http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf
- Brawley OW. Trends in prostate cancer in the United States. J Natl Cancer Inst Monogr 2012;2012:152-6.
- Rabow MW, Lee MX. Palliative care in castrate-resistant prostate cancer. Urol Clin North Am 2012;39:491-503. [PubMed]
- Paller CJ, Antonarakis ES. Management of biochemically recurrent prostate cancer after local therapy: evolving standards of care and new directions. Clin Adv Hematol Oncol 2013;11:14-23. [PubMed]
- Saad F, Miller K. Treatment options in castration-resistant prostate cancer: Current therapies and emerging docetaxel-based regimens. Urol Oncol 2013. [Epub ahead of print]. [PubMed]
- Torvinen S, Färkkilä N, Sintonen H, et al. Health-related quality of life in prostate cancer. Acta Oncol 2013;52:1094-101. [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;302:741-9. [PubMed]
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med 2008;11:180-90. [PubMed]
- Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319-26. [PubMed]
- Yennurajalingam S, Atkinson B, Masterson J, et al. The impact of an outpatient palliative care consultation on symptom burden in advanced prostate cancer patients. J Palliat Med 2012;15:20-4. [PubMed]
- Rabow M. #411-A. Presented at 2011 Annual Assembly of the American Academy of Hospice and Palliative Medicine: Feb 16-19, 2011 in Vancouver, Canada.
- Dalal S, Palla S, Hui D, et al. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist 2011;16:105-11. [PubMed]


