Metabolic syndrome and nephrolithiasis
Introduction
Nephrolithiasis is an increasingly common condition in the United States (US). Using a representative sample of the US, a recent estimate from the National Health and Nutrition Examination Survey (NHANES) reported the prevalence of a history of kidney stones of 10.6% in men and 7.1% in women with the overall prevalence increasing from 3.8% [1976-1980] to 8.8% [2007-2010] (1). Recent large scale epidemiologic studies have shown an increased prevalence of kidney stones in patients with lifestyle-related diseases such as hypertension (HTN) (2,3), diabetes mellitus (DM) (4), obesity (5) and dyslipidemia (DL). Taken together these inter-related risk factors are termed metabolic syndrome (MS). Specifically, the American Heart Association and National Heart, Lung, and Blood Institute statement consider MS if three of the following traits are present: abdominal obesity (waist circumference >102 cm in men and >88 cm in women), increased serum triglyceride level [>150 mg/dL (>169 mmol/L)] or decreased serum high-density lipoprotein (HDL) cholesterol level [<40 mg/dL (<1.03 mmol/L) in men and <50 mg/dL (<1.29 mmol/L) in women], HTN (systolic blood pressure >130 mmHg or diastolic blood pressure >85 mmHg), and DM [fasting glucose >100 mg/dL (>5.55 mmol/L)] (6). Large scale studies have shown that patients with MS seem to carry an elevated risk of atherosclerotic cardiovascular (CV) disease and all-cause mortality (7,8).
Aggregate evidence suggests kidney stone formation is increasingly prevalent in people with MS (9). This association seems to be reciprocal in nature as stone formers seem to harbor MS and ones with MS are at increased risk for kidney stones (10). We herein review the associations of CV disease, MS and its individual components and their associative risk of nephrolithiasis.
CV disease and association with nephrolithiasis
Nephrolithiasis is more prevalent in patients with MS (9,11-13). This is a growing concern as over 25% of the US population is afflicted with this systemic disorder that leads to pathologic vascular disease and atherosclerosis, and consequently, individuals with kidney stones have been demonstrated to be at increased risk for CV disease in contemporary studies. The Coronary Artery Risk Development in Young Adults (CARDIA) study is a US population-based observational study of 5,115 adults who were between the ages of 18 and 30 years, which demonstrated that young adults who form kidney stones have a higher prevalence of subclinical atherosclerosis (10). The authors measured risk factors including carotid artery intimal wall thickness, which is directly associated with CV events. After 20 years, 3.9% of patients reported having a symptomatic kidney stone. After controlling for risk factors, the development of a symptomatic kidney stone was associated with an increased risk of having carotid artery atherosclerosis (OR 1.6) (10,14).
There are other well documented associations between urinary stone formation and vascular pathology. Rule et al. reported the results of the Olmstead County study cohort in 4,564 stone formers as compared to 10,089 in non-stone formers. After adjusting for demographics, the hazard ratio (HR) for having a myocardial infarction (MI) was 1.31, which increased to 1.35 when adjusting for co-morbidities during mean follow-up of 9 years. This increased risk was independent of other common risk factors for MI (15). Eisner and colleagues also found that MI (RR—1.78), angina (RR—1.63), and congestive heart failure (RR—2.2) all occurred significantly more often in women with a history of nephrolithiasis in a study of over 10,000 women (16).
MS and risk of nephrolithiasis
There is growing epidemiologic evidence to indicate that the clustering of individual traits in MS (HTN, DM, obesity, DL) increases the severity of stone formation in affected patients (Summarized in Table 1). West et al. recently reported their findings from NHANES III, which was designed to be a probability sample of the total civilian non-institutionalized population. They collected health and nutritional data for 33,994 men, women, and children from 1988 to 1994 and found that of all adults older than 20 years, 4.7% reported a history of kidney stones. The prevalence of stones increased with the number of MS traits from 3% with zero traits to 7.5% with three traits to 9.8% with five traits. After adjustment for covariates, the presence of two or more traits significantly increased the odds of stones. The presence of four or more traits was associated with an approximate two-fold increase in odds of stone. The trait with the greatest frequency independent of the number of other traits present was HTN, which was present in 28.2% of those with one, 45.6% with two, 71.1% with three, 87.6% with four and 100% with five traits (12).
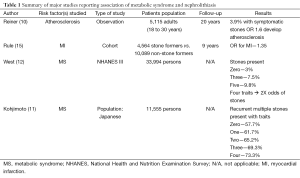
Full table
This troubling trend is ubiquitous as Kohjimoto et al. found similar findings in a large Japanese cohort. They studied 11,555 Japanese patients with some or all traits of MS. Proportions of patients with recurrent and/or multiple stones were 57.7%, 61.7%, 65.2%, 69.3%, and 73.3% with zero, one, two, three, and four MS traits, respectively (P<0.001). There was a significant and stepwise increase in the odds of recurrent and/or multiple stones even after adjustment for age and sex. Patients with four MS traits were 1.8 times more likely to be afflicted with stones than patients with zero traits (OR 1.78). The presence of any MS trait was associated with having hypercalciuria, hyperuricosuria, hyperoxaluria, and hypocitraturia after adjustment for age and sex (11). Rendina et al. recently reported that MS was associated with a 2-fold higher level of evidence of kidney stones in 2,132 inpatients in Southern Italy (17). Furthermore, Jeong et al. reported that the presence of MS had an OR of 1.25 for kidney stone prevalence using imaging in 34,895 individuals who underwent general health screening tests in Korea (18).
Evidence suggests that nephrolithiasis is indeed a systemic disease. We will now review the association of the individual components of MS and nephrolithiasis and discuss possible physiochemical and pathogenic mechanisms behind this provocative association (major studies are summarized in Table 2).
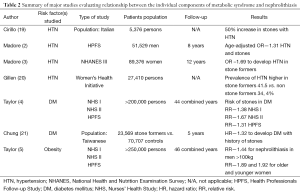
Full table
HTN and risk of nephrolithiasis
People with HTN (approximately 43 million affected adults in the US) are disproportionally affected by kidney stones compared to normotensive individuals—some prospective data suggest that a history of nephrolithiasis is associated with a greater tendency to develop HTN (4,5,22). Tibblin first reported this association in 1967 in a study of Swedish middle-aged men. Among these men, 6.5% had kidney stones based on radiographic or historical evidence. When the patients were stratified by blood pressure into four groups, the prevalence of nephrolithiasis increased from 1.1% in the lowest blood pressure group (<145/90 mmHg untreated) to 13.3% in the subjects with the highest blood pressure group (>175/115 mmHg or treated HTN) (23). Cirillo et al. reported results from the Gubbio Study—a population-based Italian survey on HTN (defined as diastolic pressure falling within the fifth quintile for each sex and age-specific category, and/or under regular antihypertensive treatment) involving 5,376 subjects. Incidence of kidney stones (radiographic and/or surgical evidence, and/or stone excretion) was increased by over 50% (P<0.01) in treated and untreated patients with HTN (19).
In the Olivetti Prospective Study of 688 men aged 21 to 68 in Italy, Cappuccio et al. found that overall prevalence of history of kidney stones was 16.3% (112/688). The relative risk (RR) of hypertensive subjects having a history of kidney stones was twice that of the normotensive group (OR 2.11). The risk was higher when only treated hypertensive men were considered (OR 3.16). The age-adjusted RR in treated hypertensive men was higher than in the normotensive group (OR 2.63) (24). A follow-up study by the same authors after eight years demonstrated that the RR was unaffected by the exclusion of treated HTN men (RR—2.01), and after adjustment for age (RR—1.89), weight (RR—1.78) or height (RR—2.00). They concluded that HTN in middle-aged men is a significant predictor of nephrolithiasis rather than a consequence of renal damage caused by the stones themselves (25). One must note that a significant number of patients (25%) were lost to follow-up, so some bias must be considered. Between 1984 and 1991, Borghi and colleagues studied 132 patients with stable essential HTN (diastolic blood pressure of more than 95 mmHg) without stone disease and 135 normotensive subjects (diastolic blood pressure less than 85 mmHg) and found that HTN patients were significantly more likely to experience stone episodes (14.3% vs. 2.9%; OR 5.5) (26).
Larger population based epidemiologic studies in the US have demonstrated the association of HTN and stones. The results of the Nurses’ Health Study (NHS) I demonstrated that the age-adjusted RR for the development of incidental HTN was 1.24 among those with a history of nephrolithiasis, as opposed to no increased risk of incidence of stones in those with no baseline HTN (3). Madore et al. reported interesting findings from an analysis of the Health Professionals Follow-up Study (HPFS). Men with a history of kidney stones were at increased risk of developing HTN, and the incident stone risk was higher in those with HTN. Analysis of initial responses to the mailed questionnaires revealed an age-adjusted OR of 1.31, between HTN (defined as systolic >139, or diastolic >89 mmHg) and nephrolithiasis in a cross-sectional analysis. Follow-up after eight years suggested that a history of nephrolithiasis corresponded with a greater tendency to develop HTN (OR 1.29). Unexpectedly, hypertensive patients did not have a higher incidence of new stones (OR 0.99) (2). In another analysis of the NHANES III, the OR of female stone formers developing HTN was 1.69 and this appeared to be increased in stone forming women with higher body mass index (BMI) (20). Interestingly, these trends were not demonstrated in the male cohort. Hall et al. investigated a large cohort of 27,410 women participating in the Women’s Health Initiative Study and found that the prevalence of HTN was significantly higher in those with nephrolithiasis as compared with non stone formers; 41.5% vs. 34.4% (27). These studies in total suggest that either nephrolithiasis predisposes to HTN, or more likely, whatever physiologic and vascular mechanisms contribute to HTN in life may also favor formation of nephrolithiasis.
DM and the risk of nephrolithiasis
Kidney stone formation and the development of DM may share common pathophysiologic pathways—it appears to be a bidirectional risk association between them (21). The most compelling evidence stems from the large epidemiological studies—the NHS I (older women) & II (younger women) and the HPFS (men). Taylor et al. analyzed these large cohorts that included over 200,000 participants over a combined 44 years of follow-up. They found that multivariate RR of stone disease in individuals with DM compared to individuals without was 1.38 in older women, 1.67 in younger women, and 1.31 in men. Prospectively, the multivariate RR of incident stone formation in participants with DM compared to participants without was 1.29 in older women and 1.60 in younger women. Interestingly men did not have an elevated risk of stone formation with only a RR of 0.81. DM was positively associated with nephrolithiasis, independent of age, BMI, thiazide use, and diet (4). The lack of association of stone formation in the male cohort could be explained due to the older age (nearly 61 years) of diabetics in the male cohort at the start of the study. Insulin resistance and compensatory hyperinsulinemia can precede the diagnosis of DM type 2 by decades, and because they excluded men with a history of stones at baseline, the prospective analysis may have excluded DM men who were likely to form stones (28).
The risk of a stone former developing DM has also been investigated. Chung et al. compared 23,569 patients with new diagnoses of kidney stones with 70,707 matched persons and followed for five years for a subsequent diagnosis of DM. Controlling for HTN, HL and obesity, the HR of receiving a first diagnosis of DM during the 5-year follow-up was 1.32 times greater for persons with stones (P<0.001). The authors suggest that persons who have kidney stones are at higher risk of developing DM within five years (21). Ando et al. investigated 1,036 (529 men and 507 women) healthy Japanese subjects, aged 35-79 years, to identify a relationship between insulin resistance and stone formation. The authors observed a significant positive trend in the age-adjusted OR for a history of stones across all insulin tertiles (P=0.04) in women (29). The authors suggest that the components of MS could increase the risk of kidney stones through subclinical hyperinsulinemia and insulin resistance.
Because urolithiasis is unlikely to cause DM directly, the positive reciprocal association between stones and DM suggests that a common metabolic defect may contribute to the development of both diseases. Several mechanisms have been suggested to explain these observations. Canda and Isgoren observed decreased function of interstitial cells and neural tissue within the urothelial tissue of diabetic rabbits and they suggested that these perturbations of function could affect ureteral peristalsis and promote urinary stone formation by virtue of urinary stasis (30). A more accepted pathway seems to be the insulin resistance seen in DM as the underlying mechanism through which stones form. Insulin resistance has been noted to impair renal ammoniagenesis, which results in acidic urine (31,32). Insulin resistance is also associated with high levels of plasma free fatty acids, which can enter the proximal tubule cells and interfere with the utilization of glutamine in the production of ammonium (33). Insulin also plays an important role in renal acidification by increasing the production of ammonium; thereby insulin resistance is associated with an impaired ability to excrete an acid load (34). We also know that a low urinary pH plays a major role in the formation of uric acid (UA) kidney stones (32,35), but a defect in renal acid excretion also could lead to hypocitraturia, an important risk factor for calcium stones (36). Furthermore, the compensatory hyperinsulinemia of insulin resistance may increase the urinary excretion of calcium (37).
Stone formers are more likely to take thiazide diuretics and these medications may increase the risk of hyperglycemia and DM type 2 (38). And finally hyperglycemia, which is a constant in DM, has been associated with increased urinary calcium and oxalate excretion, resulting in a greater risk of stone formation (39,40). Taken together, these metabolic changes may explain the consistent and bidirectional association seen between DM and nephrolithiasis.
DL and risk of nephrolithiasis
DL is defined as a disorder of lipoprotein metabolism, including lipoprotein overproduction or deficiency, which may be manifested by elevation of the total cholesterol, LDL and the triglyceride concentrations, and a decrease in HDL concentration (6). Data supporting a direct link between DL and kidney stone formation are limited. DL and stones are associated because of their mutual relatedness with insulin resistance and MS (41,42). Recently, esterified cholesterol has been implicated in the pathogenesis of atherosclerotic plaque formation and CV insult (43). Stoller et al. investigated this association in using cholesterol extraction studies on calcium oxalate stones. The authors found that esterified cholesterol accounted for 14% to 16% of total cholesterol in stones, and the esterified-to-free cholesterol ratio appeared to be related tostonecomposition. The cholesterol component of kidney stones may result from plasma leakage of free cholesterol from the vasculature (44). This provides some interesting theories to investigate, but the limited evidence suggests that DL is likely only a small part of the larger, more complex dynamic relationship between MS and stones.
Obesity and risk of nephrolithiasis
Obesity is defined as a BMI of greater than 30 kg/m2. In the United States, there has been a significant increase in obesity and its complications. The rate of obesity is alarmingly climbing as 35.7% of US adults in 2010 were obese (45-47), while the prevalence of kidney stones has also been on the rise (48). The large epidemiological studies (NHS I, II, and HPFS) have reported that obese patients have a higher risk of nephrolithiasis. Some also suggest that body size is associated with the risk of stone formation and that the magnitude of risk may even vary by gender (5,49).
Taylor and Curhan investigated this link between obesity and nephrolithiasis using combined data collected from the NHS I, II and HPFS—results from over 250,000 individuals with over 46 years of combined follow-up. After adjusting for age, dietary factors, fluid intake, and thiazide use, the RR for nephrolithiasis in men weighing more than 220 lb (100.0 kg) versus men less than 150 lb (68.2 kg) was 1.44 (P=0.002). In older and younger women, RRs for these weight categories were 1.89 (P<0.001) and 1.92 (P<0.001), respectively. They also found significantly higher risk of kidney stones in persons who progressively gained weight in adulthood and increasing BMI and waist circumference was significantly associated with risk of stone formation, with the greatest magnitude in women (5,49). In a German study, Siener et al. found that 49.6% of the 363 men and 33.5% of the 164 women with idiopathic CO stones were either overweight or obese. The obese patients (BMI >30) with stones in their population were 9.6% of the men and 10.4% of the women (50). In a French study, Daudon et al. found that of 672 recurrent KS formers, 27.1% of male and 19.6% of female stone formers were overweight, and 8.4% and 13.5% were obese, respectively (51). Obese persons also suffer from recurrent kidney stones. Lee et al. followed 163 stone-formers for more than 36 months and found that recurrence was more common in obese (42.6%) compared with non-obese stone formers (14.9%), but this was only true in first-time stone formers and not in recurrent stone formers.
Several investigators have studied urinary compositions of overweight and obese kidney stone formers. Ekeruo et al. reported that the most common presenting metabolic abnormalities among these obese patients included gouty diathesis (54%), hypocitraturia (54%) and hyperuricosuria (43%), which presented at levels that were significantly higher than those of the non-obese stone formers (P<0.05). The authors noted that after initiating treatment with selective medical and lifestyle modifications, obese and non-obese patients demonstrated normalization of metabolic abnormalities, resulting in an average decrease in new stone formation from 1.75 to 0.15 new stones formed per patient per year in both groups (52). In the large epidemiological studies, Taylor et al. also noted increased urinary excretion of oxalate, UA, phosphate, sodium, sulfate, and cysteine in obese versus non-obese patients (5). Urinary composition in the obese population seems to contain higher levels of substances known to be lithogenic compared with the non-obese population (53). Not surprisingly, weight loss and reduction of BMI has shown to reverse the metabolic derangements of MS. Dietary instructions and lifestyle guidance are valuable tools for the prevention of stone recurrence (7). Conversely, weight loss surgery (gastric bypass, not gastric banding) has actually been shown to increase the risk of stone formation, indicating that this is truly a complex, systemic derangement (54).
A direct relationship exists between obesity and nephrolithiasis, and there is growing concern considering the increasing rates of obesity in the US. Some mechanistic theories have been revealed, but much is still unknown.
UA stones and MS
UA is the end product of purine metabolism in humans who display serum and urinary UA concentrations significantly higher than other mammals. Since urinary excretion of UA in humans generally exceeds 600 mg/day, the limited urinary UA solubility of 96 mg/L poses a great risk for UA precipitation (35,55). While UA stones constitute only a minority of all nephrolithiasis cases, they are significantly more common among kidney stone formers with MS. Acidic urine is recognized as the major abnormality responsible for UA nephrolithiasis.
There is an inverse relationship between increasing BMI, insulin resistance, DM and urinary pH—in other words, urinary pH is inversely related to the number of MS traits, a finding recently reported by several investigators (4,5,31,32,34,35,56,57). Daudon et al. reported the results of an interesting French study on a large series of calculi, which examined the relationship between body size and the composition of the stones in order to assess the association of stone type and body weight. Among 18,845 consecutive calculi referred to the laboratory, 1,931 calcium oxalate or UA stones were recorded from 2,100 patients with known height and body weight. In males, the proportion of calcium oxalate stones was lower in overweight and obese groups than in normal BMI group, whereas the proportion of UA stones gradually increased with BMI, from 7.1% in normal BMI to 28.7% in obese subjects (P<0.0001). The same was true in females, with a proportion of UA rising from 6.1% in normal BMI to 17.1% in obese patients (P=0.003). Of note, the proportion of UA stones markedly rose with age in both genders as well (P<0.0001). The authors concluded that increasing body weight and mass is associated with a higher proportion of UA stones in kidney stone formers (51).
Besides a lower urinary pH, studies suggest insulin resistance, a hallmark of MS, contributes to UA nephrolithiasis. Insulin stimulates the synthesis of ammonia in the kidney and reduced ammoniagenesis in insulin-resistant states could lead to decreased urinary ammonia excretion (32). Studies of UA stone formers, however, demonstrate a lower proportion of net acid excretion in the form of ammonium, but absolute net acid excretion is not lower. The relative contribution of titratable acid to net acid excretion is increased, resulting in a lower urine pH (31,34,35). Daudon et al. found UA stones comprised 35.7 and 11.3% of stones in patients with and without DM type 2, respectively (P<0.0001). Among UA stone formers, 27.8% had DM, compared to 6.9% of calcium stone formers (P<0.0001) (56). In one high volume academic stone center, 63% of stones in obese patients were composed of UA compared to 11% in the non-obese patients (52). Lower urinary pH promoting UA stone formation may be caused by the greater ingestion, or greater endogenous production, of acid, less ingestion of dietary alkali, or reductions in urinary buffers owing to hypocitraturia (55). Data gathered from both animal models and human studies suggest that HTN also lowers urinary pH independently of BMI or DM status, which would further predispose people with these individual traits of the MS to UA stone formation (58-62).
Chronic inflammation and the pathogenesis of nephrolithiasis
Well known is the role of oxidative stress (OS) in development of CV diseases, including HTN, DM, atherosclerosis and MI (63,64). In recent years studies have linked MS and its individual components to systemic inflammation and subsequent development of atherosclerosis (7,65,66). Owing to the dynamic and complex causal relationship between MS and nephrolithiasis, investigating the role of inflammation in lithogenesis is a stimulating one.
There is an intimate relationship between CV disease and inflammatory cytokines. An inflammatory state is critical in the development of atherosclerosis, leading to the formation and propagation of complex plaques in the systemic vasculature (67-69). Extrapolating this to the microenvironment of the kidney, a pro-inflammatory state seems to exist as some investigators have found presence of molecules generally involved in inflammatory pathways, such as osteopontin, heavy chain of inter-alpha-inhibitor, collagen, and zinc in the nephron, specifically in interstitial plaques of the renal papillae in stone formers (70-75). Baggio and colleagues discovered higher than normal levels of renal enzymes, gamma-glutamyl transpeptidase (GGTP), angiotensin-1 converting enzyme (ACE), b-galactosidase (GAL), and N-acetyl-b-glucoseaminidase (NAG) in the urine of stone formers. These inflammatory markers may indicate urothelial injury, which has been postulated to increase crystal adhesion (76).
Both clinical and experimental investigations indicate that reactive oxygen species (ROS) and OS leads to inflammation (77). Investigators have offered that kidney stone formation may follow a similar pathway. They found that urine from stone forming patients had increased NAG and significantly higher a-glutathione S-transferase (a-GST), malondialdehyde (MDA) and thiobarbituric acid-reactive substances (78-80). NADPH oxidase is a major source of ROS in the kidneys.
Just as OS is intimately involved in atherosclerosis, in the microenvironment of the kidneys, stress seems to be important in the development of stones—even more in the kidneys of stone forming patients. This relationship seems bidirectional. Stress produced by one disorder may trigger the other under the right circumstances. Further research must be performed to clarify this theory further, as this likely represents one of multiple pathways in the pathogenesis of stone disease in patients with MS.
The role of antioxidants in kidney stone disease
A thought-provoking argument can be made for inflammation being a key component in lithogenesis because statins, a class of drugs developed for the purpose of interfering with the biosynthesis of cholesterol and reducing CV risk, may reduce stone risk by a novel and unsuspected anti-inflammatory and anti-oxidant role completely unrelated to cholesterol manipulation (81). In a study investigating the impact of statins on stone formation in hyperlipidemic patients, Sur et al. reported the results of 57,232 military subjects with hyperlipidemia and 1,904 subjects with nephrolithiasis. Patients taking any statin medication had significantly less stone disease compared to patients not taking statins (3.1% vs. 3.7%, OR 0.83, P<0.001). Statins had a protective effect against kidney stone formation (OR 0.51, P<0.001), after adjusting for age, sex, and co-morbidities indicating that the risk of nephrolithiasis was attenuated with the addition of statin use. It is important to note that patients on statins were more likely to have some or all traits of MS (82).
Holoch and Tracy investigated the self-reported history of nephrolithiasis and use of antioxidants in the NHANES III. After adjusting for covariates, mean levels of alpha-carotene, beta-carotene, and beta-cryptoxanthin (known antioxidants) were significantly lower in those with kidney stones (–9.36%, –10.79%, and –8.48%, respectively). When analyzed by quartile, higher serum levels of beta-carotene and beta-cryptoxanthin trended toward a decreasing prevalence of stones (P=0.007 and P=0.03, respectively), indicating that the highest levels of these antioxidants may protect against stone formation (83).
Using a rat model, Tsujihata et al. found that urinary levels of biomarkers for renal tubular cell injury, NAG and OS (8-hydroxy-2' deoxyguanosine) were decreased significantly by atorvastatin treatment. Furthermore, atorvastatin treatment decreased the apoptosis of renal tubular cells. They found that the administration of atorvastatin to stone forming rats significantly lowered crystalline deposits on quantitative light microscopy analysis of kidney specimens. The investigators hypothesized that anti-inflammatory and anti-oxidative effects of the drug were responsible, through preventing renal tubular cell injury from oxalate and subsequently inhibiting renal crystal retention and stone formation (84,85). These results provide more support that a pro-inflammatory state may be an important mediator of stone formation. Given the association between CV disease, MS and chronic inflammation, the use of antioxidants, especially statins, which have proven benefit in reducing CV morbidity and mortality in patients with MS, must be further studied to assess their efficacy in preventing nephrolithiasis in this high-risk group.
Conclusions
Increasing evidence suggests that synergistic effects of the components of MS lead to an increased risk of kidney stone disease. Therefore, the pathophysiology explaining increased stone risk related to MS likely goes beyond simple cumulative effects on urine chemistry by the individual traits of the syndrome, indicating complex and dynamic shared systemic influences likely at play. One unifying theory such as common systemic malfunction of inflammation and tissue damage as an underlying mechanism is a possibility, but it is unlikely to be the only mechanistic explanation. Further research is needed to investigate this and other hypotheses that go beyond population based and urine physiochemical studies in order to elucidate the mechanisms behind the individual disease states themselves.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scales CD Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol 2012;62:160-5. [PubMed]
- Madore F, Stampfer MJ, Rimm EB, et al. Nephrolithiasis and risk of hypertension. Am J Hypertens 1998;11:46-53. [PubMed]
- Madore F, Stampfer MJ, Willett WC, et al. Nephrolithiasis and risk of hypertension in women. Am J Kidney Dis 1998;32:802-7. [PubMed]
- Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int 2005;68:1230-5. [PubMed]
- Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA 2005;293:455-62. [PubMed]
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735-52. [PubMed]
- Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005;365:1415-28. [PubMed]
- Hong Y, Jin X, Mo J, et al. Metabolic syndrome, its preeminent clusters, incident coronary heart disease and all-cause mortality--results of prospective analysis for the Atherosclerosis Risk in Communities study. J Intern Med 2007;262:113-22. [PubMed]
- Lange JN, Mufarrij PW, Wood KD, et al. The association of cardiovascular disease and metabolic syndrome with nephrolithiasis. Curr Opin Urol 2012;22:154-9. [PubMed]
- Reiner AP, Kahn A, Eisner BH, et al. Kidney stones and subclinical atherosclerosis in young adults: the CARDIA study. J Urol 2011;185:920-5. [PubMed]
- Kohjimoto Y, Sasaki Y, Iguchi M, et al. Association of metabolic syndrome traits and severity of kidney stones: results from a nationwide survey on urolithiasis in Japan. Am J Kidney Dis 2013;61:923-9. [PubMed]
- West B, Luke A, Durazo-Arvizu RA, et al. Metabolic syndrome and self-reported history of kidney stones: the National Health and Nutrition Examination Survey (NHANES III) 1988-1994. Am J Kidney Dis 2008;51:741-7. [PubMed]
- Domingos F, Serra A. Nephrolithiasis is associated with an increased prevalence of cardiovascular disease. Nephrol Dial Transplant 2011;26:864-8. [PubMed]
- O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 1999;340:14-22. [PubMed]
- Rule AD, Roger VL, Melton LJ 3rd, et al. Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol 2010;21:1641-4. [PubMed]
- Eisner BH, Cooperberg MR, Kahn AJ, et al. Nephrolithiasis and the risk of heart disease in older women in the Study of Osteoporotic Fractures. J Urol 2009;181:517-8.
- Rendina D, De Filippo G, Mossetti G, et al. Relationship between metabolic syndrome and multinodular non-toxic goiter in an inpatient population from a geographic area with moderate iodine deficiency. J Endocrinol Invest 2012;35:407-12. [PubMed]
- Jeong IG, Kang T, Bang JK, et al. Association between metabolic syndrome and the presence of kidney stones in a screened population. Am J Kidney Dis 2011;58:383-8. [PubMed]
- Cirillo M, Laurenzi M. Elevated blood pressure and positive history of kidney stones: results from a population-based study. J Hypertens Suppl 1988;6:S485-6. [PubMed]
- Gillen DL, Coe FL, Worcester EM. Nephrolithiasis and increased blood pressure among females with high body mass index. Am J Kidney Dis 2005;46:263-9. [PubMed]
- Chung SD, Chen YK, Lin HC. Increased risk of diabetes in patients with urinary calculi: a 5-year followup study. J Urol 2011;186:1888-93. [PubMed]
- Hamano S, Nakatsu H, Suzuki N, et al. Kidney stone disease and risk factors for coronary heart disease. Int J Urol 2005;12:859-63. [PubMed]
- Tibblin G. A population study of 50-year-old men. An analysis of the non-participation group. Acta Med Scand 1965;178:453-9. [PubMed]
- Cappuccio FP, Strazzullo P, Mancini M. Kidney stones and hypertension: population based study of an independent clinical association. BMJ 1990;300:1234-6. [PubMed]
- Cappuccio FP, Siani A, Barba G, et al. A prospective study of hypertension and the incidence of kidney stones in men. J Hypertens 1999;17:1017-22. [PubMed]
- Borghi L, Meschi T, Guerra A, et al. Essential arterial hypertension and stone disease. Kidney Int 1999;55:2397-406. [PubMed]
- Hall WD, Pettinger M, Oberman A, et al. Risk factors for kidney stones in older women in the southern United States. Am J Med Sci 2001;322:12-18. [PubMed]
- Beck-Nielsen H, Vaag A, Poulsen P, et al. Metabolic and genetic influence on glucose metabolism in type 2 diabetic subjects--experiences from relatives and twin studies. Best Pract Res Clin Endocrinol Metab 2003;17:445-67. [PubMed]
- Ando R, Suzuki S, Nagaya T, et al. Impact of insulin resistance, insulin and adiponectin on kidney stones in the Japanese population. Int J Urol 2011;18:131-8. [PubMed]
- Canda AE, Isgoren AE. Re: Increased risk of diabetes in patients with urinary calculi: a 5-year followup study: S.-D. Chung, Y.-K. Chen and H.-C. Lin J Urol 2011; 186: 1888-93. J Urol 2012;187:2279-80. [PubMed]
- Sakhaee K, Maalouf NM. Metabolic syndrome and uric acid nephrolithiasis. Semin Nephrol 2008;28:174-80. [PubMed]
- Sakhaee K, Adams-Huet B, Moe OW, et al. Pathophysiologic basis for normouricosuric uric acid nephrolithiasis. Kidney Int 2002;62:971-9. [PubMed]
- Bagnasco SM, Gaydos DS, Risquez A, et al. The regulation of renal ammoniagenesis in the rat by extracellular factors. III. Effects of various fuels on in vitro ammoniagenesis. Metabolism 1983;32:900-5. [PubMed]
- Abate N, Chandalia M, Cabo-Chan AV Jr, et al. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int 2004;65:386-92. [PubMed]
- Maalouf NM. Metabolic syndrome and the genesis of uric acid stones. J Ren Nutr 2011;21:128-31. [PubMed]
- Hamm LL. Renal handling of citrate. Kidney Int 1990;38:728-35. [PubMed]
- Shimamoto K, Higashiura K, Nakagawa M, et al. Effects of hyperinsulinemia under the euglycemic condition on calcium and phosphate metabolism in non-obese normotensive subjects. Tohoku J Exp Med 1995;177:271-8. [PubMed]
- Andersson OK, Gudbrandsson T, Jamerson K. Metabolic adverse effects of thiazide diuretics: the importance of normokalaemia. J Intern Med Suppl 1991;735:89-96. [PubMed]
- Lemann J Jr, Piering WF, Lennon EJ. Possible role of carbohydrate-induced calciuria in calcium oxalate kidney-stone formation. N Engl J Med 1969;280:232-7. [PubMed]
- Eisner BH, Porten SP, Bechis SK, et al. Diabetic kidney stone formers excrete more oxalate and have lower urine pH than nondiabetic stone formers. J Urol 2010;183:2244-48. [PubMed]
- Paolisso G, Barbagallo M, Petrella G, et al. Effects of simvastatin and atorvastatin administration on insulin resistance and respiratory quotient in aged dyslipidemic non-insulin dependent diabetic patients. Atherosclerosis 2000;150:121-7. [PubMed]
- Milionis HJ, Kakafika AI, Tsouli SG, et al. Effects of statin treatment on uric acid homeostasis in patients with primary hyperlipidemia. Am Heart J 2004;148:635-40. [PubMed]
- Kruth HS. Histochemical detection of esterified cholesterol within human atherosclerotic lesions using the fluorescent probe filipin. Atherosclerosis 1984;51:281-92. [PubMed]
- Stoller ML, Meng MV, Abrahams HM, et al. The primary stone event: a new hypothesis involving a vascular etiology. J Urol 2004;171:1920-24. [PubMed]
- Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491-7. [PubMed]
- Flegal KM. Epidemiologic aspects of overweight and obesity in the United States. Physiol Behav 2005;86:599-602. [PubMed]
- Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998;22:39-47. [PubMed]
- Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int 2003;63:1817-23. [PubMed]
- Curhan GC, Willett WC, Rimm EB, et al. Body size and risk of kidney stones. J Am Soc Nephrol 1998;9:1645-52. [PubMed]
- Siener R, Glatz S, Nicolay C, et al. The role of overweight and obesity in calcium oxalate stone formation. Obes Res 2004;12:106-13. [PubMed]
- Daudon M, Lacour B, Jungers P. Influence of body size on urinary stone composition in men and women. Urol Res 2006;34:193-9. [PubMed]
- Ekeruo WO, Tan YH, Young MD, et al. Metabolic risk factors and the impact of medical therapy on the management of nephrolithiasis in obese patients. J Urol 2004;172:159-63. [PubMed]
- Powell CR, Stoller ML, Schwartz BF, et al. Impact of body weight on urinary electrolytes in urinary stone formers. Urology 2000;55:825-30. [PubMed]
- Tasca A. Metabolic syndrome and bariatric surgery in stone disease etiology. Curr Opin Urol 2011;21:129-33. [PubMed]
- Maalouf NM, Cameron MA, Moe OW, et al. Low urine pH: a novel feature of the metabolic syndrome. Clin J Am Soc Nephrol 2007;2:883-8. [PubMed]
- Daudon M, Traxer O, Conort P, et al. Type 2 diabetes increases the risk for uric acid stones. J Am Soc Nephrol 2006;17:2026-33. [PubMed]
- Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am J Kidney Dis 2006;48:905-15. [PubMed]
- Batlle DC, Sharma AM, Alsheikha MW, et al. Renal acid excretion and intracellular pH in salt-sensitive genetic hypertension. J Clin Invest 1993;91:2178-84. [PubMed]
- Sharma AM, Schorr U. Salt sensitivity and insulin resistance: Is there a link? Blood pressure. Supplement 1996;1:59-63. [PubMed]
- Sharma AM, Kribben A, Schattenfroh S, et al. Salt sensitivity in humans is associated with abnormal acid-base regulation. Hypertension 1990;16:407-13. [PubMed]
- Lucas PA, Lacour B, McCarron DA, et al. Disturbance of acid-base balance in the young spontaneously hypertensive rat. Clin Sci (Lond) 1987;73:211-5. [PubMed]
- Iba A, Kohjimoto Y, Mori T, et al. Insulin resistance increases the risk of urinary stone formation in a rat model of metabolic syndrome. BJU Int 2010;106:1550-54. [PubMed]
- Harrison D, Griendling KK, Landmesser U, et al. Role of oxidative stress in atherosclerosis. Am J Cardiol 2003;91:7A-11A. [PubMed]
- Hulsmans M, Holvoet P. The vicious circle between oxidative stress and inflammation in atherosclerosis. J Cell Mol Med 2010;14:70-8. [PubMed]
- Festa A, D’Agostino R, Howard G, et al. Inflammation and microalbuminuria in nondiabetic and type 2 diabetic subjects: The Insulin Resistance Atherosclerosis Study. Kidney Int 2000;58:1703-10. [PubMed]
- Grimble RF. Inflammatory status and insulin resistance. Curr Opin Clin Nutr Metab Care 2002;5:551-9. [PubMed]
- Takahashi M. Inflammatory cytokines in the pathogenesis of atherosclerosis. Nihon Rinsho 2011;69:30-3. [PubMed]
- Young JL, Libby P, Schonbeck U. Cytokines in the pathogenesis of atherosclerosis. Thromb Haemost 2002;88:554-67. [PubMed]
- Kaehler J, Osterholz S, Patten M, et al. Cytokines in the pathogenesis of atherosclerosis. Dtsch Med Wochenschr 2002;127:94-9. [PubMed]
- Evan AP, Unwin RJ, Williams JC Jr. Renal stone disease: a commentary on the nature and significance of Randall's plaque. Nephron Physiol 2011;119:49-53. [PubMed]
- Evan AP, Weinman EJ, Wu XR, et al. Comparison of the pathology of interstitial plaque in human ICSF stone patients to NHERF-1 and THP-null mice. Urol Res 2010;38:439-52. [PubMed]
- Evan AP, Bledsoe S, Worcester EM, et al. Renal inter-alpha-trypsin inhibitor heavy chain 3 increases in calcium oxalate stone-forming patients. Kidney Int 2007;72:1503-11. [PubMed]
- Vernon HJ, Osborne C, Tzortzaki EG, et al. Aprt/Opn double knockout mice: osteopontin is a modifier of kidney stone disease severity. Kidney Int 2005;68:938-47. [PubMed]
- Evan AP, Coe FL, Rittling SR, et al. Apatite plaque particles in inner medulla of kidneys of calcium oxalate stone formers: osteopontin localization. Kidney Int 2005;68:145-54. [PubMed]
- Tzortzaki EG, Yang M, Glass D, et al. Impaired expression of an organic cation transporter, IMPT1, in a knockout mouse model for kidney stone disease. Urol Res 2003;31:257-61. [PubMed]
- Baggio B, Gambaro G, Ossi E, et al. Increased urinary excretion of renal enzymes in idiopathic calcium oxalate nephrolithiasis. J Urol 1983;129:1161-62. [PubMed]
- Manea A. NADPH oxidase-derived reactive oxygen species: involvement in vascular physiology and pathology. Cell Tissue Res 2010;342:325-39. [PubMed]
- Huang HS, Ma MC, Chen CF, et al. Lipid peroxidation and its correlations with urinary levels of oxalate, citric acid, and osteopontin in patients with renal calcium oxalate stones. Urology 2003;62:1123-28. [PubMed]
- Tungsanga K, Sriboonlue P, Futrakul P, et al. Renal tubular cell damage and oxidative stress in renal stone patients and the effect of potassium citrate treatment. Urol Res 2005;33:65-9. [PubMed]
- Boonla C, Wunsuwan R, Tungsanga K, et al. Urinary 8-hydroxydeoxyguanosine is elevated in patients with nephrolithiasis. Urol Res 2007;35:185-91. [PubMed]
- Patel TN, Shishehbor MH, Bhatt DL. A review of high-dose statin therapy: targeting cholesterol and inflammation in atherosclerosis. Eur Heart J 2007;28:664-72. [PubMed]
- Sur RL, Masterson JH, Palazzi KL, et al. Impact of statins on nephrolithiasis in hyperlipidemic patients: a 10-year review of an equal access health care system. Clin Nephrol 2013;79:351-5. [PubMed]
- Holoch PA, Tracy CR. Antioxidants and self-reported history of kidney stones: the National Health and Nutrition Examination Survey. J Endourol 2011;25:1903-8. [PubMed]
- Tsujihata M, Yoshioka I, Tsujimura A, et al. Why does atorvastatin inhibit renal crystal retention? Urol Res 2011;39:379-83. [PubMed]
- Tsujihata M, Momohara C, Yoshioka I, et al. Atorvastatin inhibits renal crystal retention in a rat stone forming model. J Urol 2008;180:2212-17. [PubMed]


