Does early orchidopexy improve fertility?
Introduction
Cryptorchidism or undescended testis (UDT) is the most common pediatric endocrine abnormality in boys. UDT is seen in 1-4.5% of newborns and is even more common in premature infants (1,2). The majority of UDT will spontaneously descend by 1 year of age such that the overall incidence becomes 0.8-1.2% (3-5), with the remaining cases usually unilateral cryptorchidism. While the exact pathophysiology of UDT remains unclear, several important sequelae of the disorder have been established with impaired fertility and increased rates of testicular malignancy being the principle among these.
Assessing fertility
The ability to definitively pronounce fertility in this population is challenging for multiple reasons. While many authors attempt to characterize “fertility potential” at the time of orchidopexy with examination of the testicular biopsy, a semen analysis later in life or proven fertility (baby in arms) are certainly better metrics. However, with the large time period elapsed between a childhood operation and adulthood, the ability to closely follow these patients in any large number is challenging and studies are plagued by bias. Indeed in one study, only 10% of the initial 200 children who underwent orchidopexy were able to be located and provide a semen analysis later in life (6). Due to this paradigm, we are frequently forced to make logical jumps in our attempts to determine if a physician’s actions taken in the first years of life will affect later fertility. While the effect of age at orchidopexy on future semen analyses has been evaluated in some studies, results are difficult to interpret as these boys had surgery frequently after 2 years of age, a time frame now outside of contemporary guidelines. By better understanding the embryology of perinatal testicular development, we can strive to improve our ability to predict future fertility in these patients.
Is the risk of infertility in cryptorchidism real?
Retrospective reviews of paternity rates have shown a fertility risk particularly in bilaterally cryptorchid men (7). However, the degree to which having one UDT affects fertility is certainly conceptually more difficult to understand assuming there is a contralateral, normal testicle. Miller et al. reported paternity rates of men with a history of unilateral UDT at 89.7%, which was not statistically different than the 93.7% found in the normal population (8). However, another examination found a larger and statistically significant difference with unilateral cryptorchid men unable to father children in 10.5% of cases, compared to only 5.4% in the control group (9). In those men that did achieve pregnancy, time to conception was not different between unilaterally cryptorchid men and controls. In concert, these studies point towards, at most, a small risk associated with unilateral UDT. However, as we will discuss later, the assumption that the contralateral testis is completely normal may not be a valid.
Embryology of normal testicular development
The human male testis contains germ cells in varying stages of development along with supporting Sertoli cells and Leydig cells in the interstitium. The primordial germ cells arise from the yolk sac and then migrate to the gonadal ridge, where they become incorporated into the sex cords. During puberty, the sex cords hollow out to form the seminiferous tubules which are lined by Sertoli cells. It is in the seminiferous tubules where spermatogenesis, or the formation of mature sperm cells, takes place. The Sertoli cells function to protect and nourish the developing sperm (10).
Two essential steps for the formation of mature sperm appear to begin pre-pubertally. The first is disappearance of gonocytes, or fetal stem cells, and the appearance of adult dark spermatogonia (AdS), the adult stem cell pool (11,12). The transformation of gonocytes into AdS begins this process and starts occurring as early as 3 months of life. Around this time, transformation appears to be under the control of a surge of gonadatropins and androgens (13) with the process generally complete by 12 months of age (14). By 3-5 years of age, the AdS will further differentiate into primary spermatocytes, as they will remain until puberty, and the onset of spermatogenesis (15,16).
Abnormal germ cell development
It appears that the transformation of gonocytes to AdS is defective in the child with UDT (11,17) with an abnormal persistence of gonocytes beyond the usual physiologic window (18). However, the causality of this relationship is unclear. There is still debate as to whether the testis is inherently developmentally defective, or if the elevated temperature (due to a lack of descent) is the causative factor. Regardless, the decreased number of developed AdS leads to inadequate future stem cells for spermatogenesis with lower sperm counts and subsequent infertility. The decision for surgery (oncologic considerations aside) assumes that this process is at least somewhat reversible and the decision to place the testis into its physiologic home in the scrotum will prevent further deterioration.
While every surgeon performing orchidopexy hopes that their efforts to descend these testicles into the scrotum will lead to a physiologically normal testicle completely contributing to future fertility, this may not be the case. In an examination of stillborn fetuses, those with cryptorchid testes had lower number of germ cells per tubule than those with normally descended testicles (19). In a different study, 72 intra-abdominal testicles were biopsied at time of orchidopexy and compared to 94 normally descended testicles. After 6 months of age, a decline was noted in spermatogonia with more pronounced effects noted at 2 years. In boys older than 3 years of age at biopsy, 64% had a complete lack of germ cells (20).
There is evidence of similar, yet often less pronounced, histological differences in the contralateral, normally descended testis signifying more than a localized, unilateral defect. While a significant impediment to transformation from gonocytes to AdS is noted in the UDT, a delay was noted also in the contralateral testis, although in most cases transformation was complete by 12 months of age (11). The lower fertility in men with unilateral UDT reported in some publications supports a more global dysfunction that is not purely limited to the UDT and an abnormal hypothalamic-pituitary axis has been postulated as the cause of contralateral testis dysfunction (13). There is certainly a correlation with global and often multisystem defects in boys with bilateral cryptorchidism (21).
Extrapolating data to predict fertility
Histological and hormonal attributes of testicular function have enabled researchers to attempt to predict fertility in men with a history of UDT. Commonly used parameters include measured testicular volume, hormone levels (FSH, LH, inhibin B, testosterone), and semen analysis. Histologic characteristics of testicular tissue taken at the time of orchidopexy have also been used to attempt to correlate future fertility.
Cell types present at orchidopexy
The number of cells, or cells per transverse section of tubule, in testicular biopsies is often used as a marker of fertility potential in cryptorchid boys (22). Hadziselimovic et al. examined testicular biopsies taken at orchidopexy between the ages of 10 months to 13 years and compared them to semen analysis done on the same patients when they were 21 to 25 years old (23). Unilateral UDT patients treated before the age of 3 years had 3-fold higher sperm counts than those treated after the age of 8. AdS were once again shown to be influential, as those without AdS at the time of orchidopexy had a 7-fold lower sperm count than those with these mature cells. A correlation between sperm concentration and number of AdS was also found. This study supports the notion that AdS are a vital component of spermatogenesis and their presence may ultimately determine future fertility potential.
The importance of the maturational transition from gonocytes to AdS was further verified in a long term study by Kraft et al. which included 110 patients (24). While the mean age at orchidopexy was 7 years, the development and preservation of AdS appeared to be the most important factor in future fertility. While severity of germ cell abnormalities was not statistically significant, the mean sperm count and sperm concentration were significantly decreased in the men with abnormal AdS development. Interestingly, despite the advanced age at orchidopexy in the study, younger age at the time of surgery was positively correlated with almost all semen analysis characteristics.
Testicular volume
The volume of the testicles at orchidopexy is often reduced the later the surgery is performed on the cryptorchid testis (25,26). However, testicular volume may not be an appropriate proxy for future fertility based on studies following paternity rates of men with cryptorchid testes. A study by Lee et al. found no relationship to testicular size at orchidopexy for unilateral UDT on future fertility as measured by actual paternity rates (27). Possible explanations for this include hypertrophy of the normally descended testicle, which could compensate for impaired fertility of the abnormal testis.
Hormonal studies
Testing for the serum levels of gonadotropin and inhibin B in blood samples of boys and determining the germ cells per tubule (GC/T) at the time of orchidopexy has also been used as a marker for fertility potential. Thorup et al. classified bilateral cryptorchid boys into groups of low, intermediate and high risk for infertility based on these parameters. They determined that boys with normal gonadotropins, inhibin B and germ cell numbers had a good fertility prognosis after surgery, while those with abnormalities in these qualities had less fertility potential (28). In a follow up study the authors noted that the group with the highest fertility potential also had the highest number of AdS (14). In examined paternity rates in men with bilateral UDT, elevated levels of FSH and LH were seen along with lower inhibin B levels, in the group with the lowest paternity rate (7).
Evidence favoring early orchidopexy
The prescribed age at which boys should undergo orchidopexy has been decreasing in the last few decades. A report from the early 1970s demonstrated a difference between the pre-pubertal testis and samples taken from boys who were in their first two years and recommended lowering the age of surgical intervention from 6 to 2 years (29). In another work from the 1970s, Ludwig et al. showed that boys who were operated on in the first two years of life had a 90% rate of fertility. This was in contrast to those boys operated on in years 3-4 (50% rate) and in those who had operations in years 9-12 (30%). While this study did not include the original position of the testicle at time of orchidopexy, a factor possibly not recognized as important at the time, these results certainly speak to a recommendation for earlier orchidopexy (30).
A randomized controlled trial comparing boys who underwent orchidopexy at either 9 months or 3 years used common fertility predicting factors as outcomes. The authors found that the number of germ cells and Sertoli cells present in the early surgery group were significantly increased compared to the group at 3 years. At both ages, testicular volume correlated to the number of germ and Sertoli cells with the early surgery group maintaining larger testicular volumes. Interestingly, hormone analysis during the first 6 months of life could not predict the cell numbers, nor could it predict testicular descent (25).
Germ cell depletion was reported from a retrospective study looking at histopathology at the time of orchidopexy. The odds for germ cell depletion were calculated relative to a group undergoing orchidopexy at less than or equal to one year. Increasing odds of cell depletion were noted with increasing age, with boys undergoing orchidopexy at 13-24 months having an odds ratio (OR) =3.9 for cell depletion, compared to those having surgery before a year of life. With each increasing age group the OR for germ cell depletion roughly doubled, reaching an OR =16.8 for boys undergoing orchidopexy at greater than 8 years of age (31). While the number of germ cells were roughly identical in the undescended and contralateral descended testis in a study by Huff et al., (18) after 12 months the cryptorchid patient was noted to have a lower overall number of AdS cells/tubule and total germ cells per tubule. Gonocyte numbers were higher in the cryptorchid testicle during the 6-18 months period, implying a lack of progression to more mature stem cell lines.
In another analysis of germ cells, boys who underwent surgery before 6 months of age were compared to those having surgery between 6 and 24 months (32). Authors were able to demonstrate a negative correlation between age at orchidopexy and germ cell counts. All of the 14 boys who had surgery before 6 months of age had a normal number of GC/T compared to the lower numbers seen in those having surgery between 6 and 24 months of age. However, the data from 20 years post-operatively called into question the use of these fertility predictors as there was no association between germ cell counts on biopsy and the total sperm count on semen analysis. Interestingly, among the boys who had surgery at less than 6 months, 31% had a sperm count less than 40 million and sperm counts between groups were not statistically different (<6 months: 136×106 sperm/ejaculate; >6 months: 96×106 sperm/ejaculate, P=0.28) despite the more frequent abnormal histology in the boys undergoing orchidopexy at greater than 6 months of life. The authors then examined results based not on patient age at orchidopexy, but on presence of AdS on biopsy. Almost all males who had developed this more mature cell line had a normal sperm count. This was in stark contrast to the group who had not undergone the transformation, wherein a majority of the men had azoospermia or oligospermia. These results are muddied by the inclusion of both unilateral and bilateral UDT in the cohort, but more clearly show that this maturational step is likely paramount to future fertility and that care decisions should be made to optimize the ability of the testicle to undergo this maturational change. In another study of testicular biopsies performed at the time of orchidopexy, a lower age at surgery was correlated with presence of spermatogonia (r=0.37, P<0.0001) and decreasing tubular atrophy (r=0.59, P<0.001) (33).
While much of the information above has shown a decreased risk for infertility in early orchidopexy according to the presence of germs cells or AdS, few studies are able to correlate these histopathologic findings, and fertility prediction assumptions, to actual paternity rates. While not entirely conclusive, these studies do point towards a decrease in potential fertility (loss of future sperm producing cells) with delayed treatment of the UDT. The point warrants reiterating that these testicles may not be inherently normal at baseline and our efforts may simply prevent further deterioration in an already pathologic testicle or testicles. As the general consensus is now that spontaneous descent is rare beyond 6 months of age (2,34,35), the optimal age to balance anesthesia risks and maximization of testicular health without operating on children who would not need surgery continues to be debated.
The new American Urological Association guidelines for orchidopexy published in 2014 are reasonable in their recommendation for surgery before 18 months of age (15). However, the surgeon should consider routinely performing the surgery before one year of age, as some boys are noted to have decreasing germ cells in the 15-18 months range (36). With this in mind, the Nordic consensus on treatment of undescended testes and the European Association of Urology, published in 2006 and 2013, respectively, advocate for surgery starting at 6 months and preferably performed by age 12 months (37,38). Table 1 provides a summary of these recommendations.
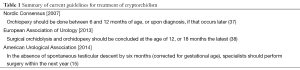
Full table
Some studies have found a critical window (likely two years of age) after which there does not appear to be a continued risk of deteriorating germ cell function (39-41), although other authors would certainly call this into question (23,24,42-44). In examination of boys undergoing unilateral orchidopexy, there was no difference in timing of surgery with regards to future fertility potential in boys operated on at 2-12 years of age (45). However, some recommendations still advise operating on the cryptorchid testis at the time of diagnosis, even if past the one year mark (37).
Future research potential
Future translational research should aim to further expand our knowledge and allow for a more nuanced approach to the proper timing of orchidopexy for fertility preservation. From the data above, it is fairly clear there is a defect in the transformation of the fetal gonocytes to AdS in these cryptorchid testicles that may not be exclusively due to their ectopic location. Additional work could focus on possible prevention strategies to reduce this malfunction in cellular development, as previous hormonal manipulation around the time of orchidopexy has been shown to improve fertility index measurements (46-48). One study was even able to demonstrate improved semen analyses later in life (49).
In particular, long term studies carefully correlating paternity in men with varying ages at orchidopexy are needed. Even more valuable information will be obtained as men who underwent early orchidopexy become of the age to have their fertility assessed. While these studies are difficult to perform due to the long time period between surgery and attempts at fertility, these data would likely be the most helpful to the urologic community in determining the ideal age of orchidopexy.
Conclusions
It has long been known that a history of cryptorchidism is associated with a reduction in future fertility. Historical studies have indicated improved fertility in earlier age at orchidopexy and surgical trends have followed with a decreasing age of both diagnosis and corrective surgery in recent years. While largely inferred from a variety of data, there is compelling evidence for early orchiopexy, although the ideal study has not yet been completed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ashley RA, Barthold JS, Kolon TF. Cryptorchidism: pathogenesis, diagnosis, treatment and prognosis. Urol Clin North Am 2010;37:183-93. [PubMed]
- Hutson JM, Balic A, Nation T, et al. Cryptorchidism. Semin Pediatr Surg 2010;19:215-24. [PubMed]
- Elder JS. The undescended testis. Hormonal and surgical management. Surg Clin North Am 1988;68:983-1005. [PubMed]
- Khatwa UA, Menon PS. Management of undescended testis. Indian J Pediatr 2000;67:449-54. [PubMed]
- Leissner J, Filipas D, Wolf HK, et al. The undescended testis: considerations and impact on fertility. BJU Int 1999;83:885-91. [PubMed]
- Fallon B, Kennedy TJ. Long-term follow-up of fertility in cryptorchid patients. Urology 1985;25:502-4. [PubMed]
- Lee PA, Coughlin MT. Fertility after bilateral cryptorchidism. Evaluation by paternity, hormone, and semen data. Horm Res 2001;55:28-32. [PubMed]
- Miller KD, Coughlin MT, Lee PA. Fertility after unilateral cryptorchidism. Paternity, time to conception, pretreatment testicular location and size, hormone and sperm parameters. Horm Res 2001;55:249-53. [PubMed]
- Lee PA, O’Leary LA, Songer NJ, et al. Paternity after unilateral cryptorchidism: a controlled study. Pediatrics 1996;98:676-9. [PubMed]
- Hadziselimovic F. eds. Cryptorchidism, management and implications. New York: Springer, 1983.
- Huff DS, Fenig DM, Canning DA, et al. Abnormal germ cell development in cryptorchidism. Horm Res 2001;55:11-7. [PubMed]
- Hutson JM. When to operate and when to investigate. Dialogues Pediatr Urol 2005;26:2-3.
- Hadziselimović F, Thommen L, Girard J, et al. The significance of postnatal gonadotropin surge for testicular development in normal and cryptorchid testes. J Urol 1986;136:274-6. [PubMed]
- Thorup J, Kvist K, Clasen-Linde E, et al. The relation between adult dark spermatogonia and other parameters of fertility potential in cryptorchid testes. J Urol 2013;190:1566-71. [PubMed]
- Kolon TF, Herndon CD, Baker LA, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol 2014;192:337-45. [PubMed]
- Huff DS, Hadziselimovic F, Snyder HM 3rd, et al. Postnatal testicular maldevelopment in unilateral cryptorchidism. J Urol 1989;142:546-8. [PubMed]
- Huff DS, Hadziselimović F, Snyder HM 3rd, et al. Early postnatal testicular maldevelopment in cryptorchidism. J Urol 1991;146:624-6. [PubMed]
- Huff DS, Hadziselimovic F, Snyder HM 3rd, et al. Histologic maldevelopment of unilaterally cryptorchid testes and their descended partners. Eur J Pediatr 1993;152 Suppl 2:S11-4. [PubMed]
- Cortes D, Thorup JM, Beck BL. Quantitative histology of germ cells in the undescended testes of human fetuses, neonates and infants. J Urol 1995;154:1188-92. [PubMed]
- Hadziselimovic F, Herzog B, Buser M. Development of cryptorchid testes. Eur J Pediatr 1987;146 Suppl 2:S8-12. [PubMed]
- Snyder HM 3rd. Bilateral undescended testes. Eur J Pediatr 1993;152 Suppl 2:S45-6. [PubMed]
- Murphy F, Paran TS, Puri P. Orchidopexy and its impact on fertility. Pediatr Surg Int 2007;23:625-32. [PubMed]
- Hadziselimovic F, Hocht B, Herzog B, et al. Infertility in cryptorchidism is linked to the stage of germ cell development at orchidopexy. Horm Res 2007;68:46-52. [PubMed]
- Kraft KH, Canning DA, Snyder HM 3rd, et al. Undescended testis histology correlation with adult hormone levels and semen analysis. J Urol 2012;188:1429-35. [PubMed]
- Kollin C, Stukenborg JB, Nurmio M, et al. Boys with undescended testes: endocrine, volumetric and morphometric studies on testicular function before and after orchidopexy at nine months or three years of age. J Clin Endocrinol Metab 2012;97:4588-95. [PubMed]
- van Brakel J, Kranse R, de Muinck Keizer-Schrama SM, et al. Fertility potential in men with a history of congenital undescended testes: a long-term follow-up study. Andrology 2013;1:100-8. [PubMed]
- Lee PA, Coughlin MT, Bellinger MF. No relationship of testicular size at orchiopexy with fertility in men who previously had unilateral cryptorchidism. J Urol 2001;166:236-9. [PubMed]
- Thorup J, Petersen BL, Kvist K, et al. Bilateral undescended testes classified according to preoperative and postoperative status of gonadotropins and inhibin B in relation to testicular histopathology at bilateral orchiopexy in infant boys. J Urol 2012;188:1436-42. [PubMed]
- Hedinger C. The moment of the earliest recognizable changes of the testicles in cryptorchidism of infants (author's transl). Verh Dtsch Ges Pathol 1971;55:172-5. [PubMed]
- Ludwig G, Potempa J. Optimal time for treating cryptorchism (author’s transl). Dtsch Med Wochenschr 1975;100:680-3. [PubMed]
- Tasian GE, Hittelman AB, Kim GE, et al. Age at orchiopexy and testis palpability predict germ and Leydig cell loss: clinical predictors of adverse histological features of cryptorchidism. J Urol 2009;182:704-9. [PubMed]
- Hadziselimovic F, Herzog B. The importance of both an early orchidopexy and germ cell maturation for fertility. Lancet 2001;358:1156-7. [PubMed]
- Canavese F, Cortese MG, Magro P, et al. Cryptorchidism: medical and surgical treatment in the 1st year of life. Pediatr Surg Int 1998;14:2-5. [PubMed]
- Hamza AF, Elrahim M. Testicular descent: when to interfere? Eur J Pediatr Surg 2001;11:173-6. [PubMed]
- Wenzler DL, Bloom DA, Park JM. What is the rate of spontaneous testicular descent in infants with cryptorchidism? J Urol 2004;171:849-51. [PubMed]
- Cortes D, Thorup JM, Visfeldt J. Cryptorchidism: aspects of fertility and neoplasms. A study including data of 1,335 consecutive boys who underwent testicular biopsy simultaneously with surgery for cryptorchidism. Horm Res 2001;55:21-7. [PubMed]
- Ritzén EM, Bergh A, Bjerknes R, et al. Nordic consensus on treatment of undescended testes. Acta Paediatr 2007;96:638-43. [PubMed]
- Tekgül S, Riedmiller H, Dogan HS, et al. Guidelines on Paediatric Urology. European Association of Urology. Paediatric Urology Update March 2013.
- Vinardi S, Magro P, Manenti M, et al. Testicular function in men treated in childhood for undescended testes. J Pediatr Surg 2001;36:385-8. [PubMed]
- Gracia J, Sánchez Zalabardo J, Sánchez García J, et al. Clinical, physical, sperm and hormonal data in 251 adults operated on for cryptorchidism in childhood. BJU Int 2000;85:1100-3. [PubMed]
- Coughlin MT, Bellinger MF, Lee PA. Age at unilateral orchiopexy: effect on hormone levels and sperm count in adulthood. J Urol 1999;162:986-8. [PubMed]
- Trsinar B, Muravec UR. Fertility potential after unilateral and bilateral orchidopexy for cryptorchidism. World J Urol 2009;27:513-9. [PubMed]
- de Gouveia Brazao CA, Pierik FH, Erenpreiss Y, et al. The effect of cryptorchidism on inhibin B in a subfertile population. Clin Endocrinol (Oxf) 2003;59:136-41. [PubMed]
- McAleer IM, Packer MG, Kaplan GW, et al. Fertility index analysis in cryptorchidism. J Urol 1995;153:1255-8. [PubMed]
- Cortes D, Thorup JM, Lindenberg S. Fertility potential after unilateral orchiopexy: an age independent risk of subsequent infertility when biopsies at surgery lack germ cells. J Urol 1996;156:217-20. [PubMed]
- Bica DT, Hadziselimovic F. Buserelin treatment of cryptorchidism: a randomized, double-blind, placebo-controlled study. J Urol 1992;148:617-21. [PubMed]
- Huff DS, Snyder HM 3rd, Rusnack SL, et al. Hormonal therapy for the subfertility of cryptorchidism. Horm Res 2001;55:38-40. [PubMed]
- Schwentner C, Oswald J, Kreczy A, et al. Neoadjuvant gonadotropin-releasing hormone therapy before surgery may improve the fertility index in undescended testes: a prospective randomized trial. J Urol 2005;173:974-7. [PubMed]
- Hadziselimović F, Herzog B. Treatment with a luteinizing hormone-releasing hormone analogue after successful orchiopexy markedly improves the chance of fertility later in life. J Urol 1997;158:1193-5. [PubMed]


