Staged urethroplasty in the management of complex anterior urethral stricture disease
Introduction
In the past, anterior urethral strictures were often repaired using a staged approach (1). Mirroring the advancements with pediatric hypospadias surgery, adult anterior urethral strictures are now more commonly managed with single stage reconstruction. However, the modern staged urethral reconstruction described by Bracka in 1995 offers a versatile approach to a variety of difficult anterior urethral strictures (2,3). Long segment strictures of the pendulous urethra may be considered for a multi-stage repair, especially in the setting of lichen sclerosus (LS), previous hypospadias repair, recurrence following prior reconstruction, or radiation therapy (4). Although single stage urethroplasty using buccal mucosa or dartos-based flaps may be used in some of these situations (5-7), the absence or severe destruction of the urethral plate and possible associated deficiencies of the adjacent penile skin make a multi-stage approach attractive. In addition, the incorporation of buccal mucosa into staged urethral reconstruction has improved outcomes considerably (8). The use of staged buccal mucosa graft urethroplasty allows replacement of nearly the entire urethra if necessary. However, the classically termed “two-stage urethroplasty” is often a misnomer as a significant number of these patients may require greater than two surgeries to yield a patent tubularized urethra (9).
Evaluation
Germaine to the evaluation of any patient presenting with a complex anterior urethral stricture is an understanding of their previous surgical interventions. Many patients have extensive urological histories and are unable to provide records, especially in the setting of prior pediatric hypospadias surgery.
Physical examination should focus on the quality and quantity of the adjacent penile skin and the possible presence of LS. If there is active inflammation related to LS, a trial of topical steroid (clobetasol topical cream, 0.05%) is warranted. Failure to improve or concerning appearance should prompt a biopsy to confirm the diagnosis and rule out malignancy if not done previously.
It is critical to stage the urethral stricture radiographically, and this is most commonly done using retrograde urethrography (RUG) with or without antegrade voiding cystourethrography (VCUG). These studies confirm the presence of a stricture, and serve to define the nature and extent for operative planning. The patient should be counseled that approximately 2-3 months of urethral rest are required before accurate diagnostic imaging can be obtained and reconstructive surgery performed. This time period is needed to allow areas that may be temporarily dilated or altered to restricture and allow accurate determination of stricture length and severity. If a patient has undergone recent endoscopic management or is requiring intermittent self-catheterization to maintain urethral patency, placement of a suprapubic catheter is discussed to allow an appropriate period of urethral rest.
Finally, a thorough discussion of the timeline and expected outcomes of a multistage urethral reconstruction should be discussed with the patient in detail. They must understand that there will be a period of a few months during which they will need to sit to void while waiting for urethral tubularization. Risks of recurrent stricture, urethral fistula, and possible need for more than two procedures are reviewed. As an alternative, especially in older patients with panurethral strictures, perineal urethrostomy is an attractive option as it relieves the obstruction in a single operative procedure with good success rates (10).
Surgical approach/technique
First stage
First stage reconstruction of the pendulous urethra is carried out in the supine position, but patients requiring simultaneous repair of a continuous or second bulbous urethral stricture are placed in the high lithotomy position to address that portion. They are then repositioned into low lithotomy using adjustable stirrups in order to proceed with the distal repair. A vertical full thickness incision into the lumen of the urethra from the meatus or distal most point of the stricture is carried out. The incision is carried proximally until healthy and patent urethra is identified. In the setting of a panurethral stricture the proximal most extent may be at the point of the previous substitution urethroplasty involving the distal bulbous urethra, and these repairs should be overlapped slightly if possible. Flexible cystoscopy is performed to evaluate the remaining urethra and bladder, and a proximal urethrostomy is created.
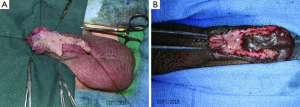
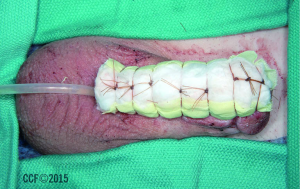
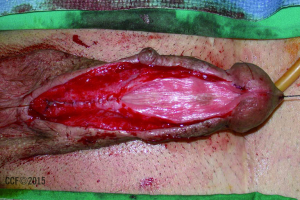
The urethral plate is examined and in areas of dense scar or unacceptable tissue quality, the plate is excised. This is most common in cases of severe LS, requiring excision of the urethra within the glans back to a centimeter or two proximal to the corona. We have observed that the remaining urethral plate often appears healthy enough to include as part of the repair and is usually left in place decreasing the quantity of buccal mucosa required. The edges of the remaining urethral plate and spongiosum are oversewn with running fine chromic suture for hemostasis. Buccal mucosa is harvested unilaterally or bilaterally based on the area needed for coverage. Often there is some adequate remaining urethral plate or acceptable substitution in the setting of previous hypospadias repair, and the graft is split and sutured in place bilaterally between the urethral plate and skin edges (Figure 1). If the distal urethra is absent the glans may be incised in the midline, or the distal urethra may require complete excision as described above for LS strictures. In these situations, we commonly split the graft into a “pair of pants” configuration. It is important to insure that the graft is wide in the glans (approximately 2.5-3 cm) to increase the chance of ultimately achieving a glanular meatus (Figure 2). Our goal is to try to achieve a urethral plate of approximately 3 cm along the entire length of the repair after the first stage is completely healed. The graft is configured to fill whatever defect is present to accomplish this (Figure 3). This will correspond to a reconstructed lumen of approximately 22-24 French at the time of second stage closure. Sutures of 4-0 and 5-0 chromic are used to secure the graft peripherally and to quilt the graft to the underlying dartos overlying the tunica. Xerofrom gauze is applied to the area, followed by a bolster dressing of artificial cotton moistened with normal saline and mineral oil is applied. Tie over sutures are used to secure the bolster in place, immobilizing the graft (Figure 4). The bolster remains in place for 5 days, and the foley catheter is removed 3 weeks postoperatively. The patient is periodically examined thereafter to assess graft take and tissue quality.


Second stage tubularization
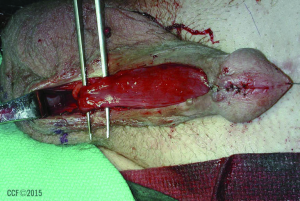
After an interval of 4-6 months depending on tissue healing, the patients progress to tubularization. Cystoscopy is performed to assess the urethrostomy and the urethra more proximally, especially in the setting of a previous proximal repair. The graft/plate width is inspected (Figure 5). The junction of the graft and penile skin is incised sharply, and a small amount of hairless genital skin may be included if needed to achieve sufficient width. Occasional insufficiency of the urethral plate may be seen near the penoscrotal junction when reconstructing a panurethral stricture related to LS, as there may not have been sufficient buccal mucosa to bridge the entire length of the stricture. We have tended to harvest lingual mucosa to be used as a ventral onlay in that location at the time of second stage closure. In other areas of the repair, additional lingual or buccal mucosa (if only one cheek was used at the initial procedure) can be harvested and placed dorsally or ventrally where needed. Augmenting the second stage closure with oral mucosa in this fashion eliminates the need for additional surgical procedures to revise first stage grafting prior to tubularization in most cases. Interrupted and running 5-0 PDS suture is used to retubularize the urethra taking care to invert the mucosa with careful needle placement (Figure 6). We attempt to achieve a meatus on the glans in most cases, using deep sutures of 4-0 or 5-0 PDS, even though in the setting of LS there may not be very much glans that can be closed ventral to the meatus without compromising luminal caliber. A layer of dartos is mobilized if possible to cover the suture line with care taken to preserve blood supply to the genital skin. A tunica vaginalis flap may be harvested if there is insufficient dartos fascia for an adequate second layer, most commonly needed in patients with a history of prior hypospadias surgery (Figure 7). The urine is diverted with a 16 French Foley catheter or using a suprapubic catheter and a urethral stent (Figure 8). A voiding cystourethrogram is performed 3 weeks postoperatively at the time of catheter or stent removal.


Outcomes
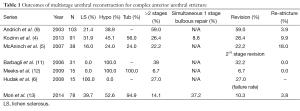
Several retrospective series have looked at a multistage urethral reconstruction for complex anterior urethral strictures involving the penile urethra. Direct comparison is often difficult due to the unique nature of each individual case. Table 1 summarizes the outcomes of these series and our most recent data.
Historically, staged urethral reconstruction using skin grafts was associated with a long-term success rate of approximately 50%. The introduction of oral mucosa grafts has had a significant favorable impact, improving overall success rates to 80% (11). In modern series, the efficacy of multistage repair for complex anterior urethral strictures is excellent, with acceptably low long-term rates of recurrent stricture ranging from 0-18%. In those studies limited to patients with a history of previous surgery for hypospadias, stricture free rates are generally superior to those that include LS patients (11,12,14), although direct comparison is difficult.
The most common complications following second stage tubularization are distal suture line dehiscence, urethrocutaneous fistula, and recurrent stricture. In our series, 78 patients underwent multistage reconstruction with an overall complication rate of 19.2% and a revision rate of 10.3%. The most common complication was urethrocutaneous fistula (7.7%), followed by glanular or distal urethral dehiscence (5.1%) and recurrent stricture requiring intervention (3.8%) (13). While it may acceptable to leave a coronal or subcoronal meatus functionally, it is usually our goal to try to provide the patient with a urethral meatus on the glans as mentioned previously, and this may explain some of the distal suture breakdown in our cohort.
Many patients undergoing staged urethral reconstruction have suffered from years of recurrent stricture and repeated interventions. Resolution of these obstructive symptoms following the initial stage offers considerable improvement to many. Elliott et al. demonstrated that as few as 24% elect to proceed with tubularization, and instead prefer to remain with a proximal urethrostomy (15). Although we have seen patients in this category as well, over 94% of our group of 78 patients progressed to tubularization (13). Although this difference is difficult to discern, it is possible that a younger or more sexually active patient population may desire tubularization which allows a more normal cosmetic outcome for the penis and upright voiding.
The classic terminology of a “2-staged” urethoplasty in this setting may be a misnomer. Some patients require an additional planned stage, such as a long segment or panurethral stricture in the setting of a concealed penis requiring a modified Cecil type procedure or scrotal flap for penile shaft skin coverage. Of previously reported patients requiring more than two surgical procedures, it seems that the majority have undergone surgical revision of the initial grafting procedure to achieve a urethral plate sufficient for tubularization. The revision rate in contemporary series ranges from 6.7% to 59% (Table 1) thus making the term “multistage” urethroplasty more apt. When feasible, it has generally been our practice to perform this augmentation or revision at the time of second stage tubularization, using oral mucosa or hairless genital skin. Kozinn et al. have suggested that the revision rate in patients with LS versus those with hypospadias failure is increased, although it did not reach statistical significance. They importantly note that up to 20% of hypospadias failure patients have evidence of LS as well (4). Our data show no significant difference in overall complications, revisions, or recurrent stricture rates between strictures related to LS and those related to failure of prior hypospadias surgery (13). However, most authors would agree that the presence of LS introduces significant surgical challenges and less favorable results, and this may be manifest with longer term follow-up.
Full table
Conclusions
Staged buccal mucosa graft urethroplasty is often necessary to manage difficult anterior urethral strictures that involve the pendulous urethra, especially in the setting of LS and those related to complications following prior surgery for hypospadias. Rates of urethral patency seem to be very good, with an acceptably low number of surgical revisions. Multistage urethroplasty should replace “2-stage” urethroplasty as the accepted terminology as it is not uncommon for patients to require more than two procedures complete successful tubularization. This may lead to more realistic patient expectations as well. Although completion of the second stage may not always necessary for functional improvement, cosmetic outcomes with restoration of a glanular meatus can be excellent and achieved in the majority of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Johanson B. The reconstruction in stenosis of the male urethra. Z Urol 1953;46:361-75. [PubMed]
- Bracka A. The role of two-stage repair in modern hypospadiology. Indian J Urol 2008;24:210-8. [PubMed]
- Bracka A. A versatile two-stage hypospadias repair. Br J Plast Surg 1995;48:345-52. [PubMed]
- Kozinn SI, Harty NJ, Zinman L, et al. Management of complex anterior urethral strictures with multistage buccal mucosa graft reconstruction. Urology 2013;82:718-22. [PubMed]
- McAninch JW, Morey AF. Penile circular fasciocutaneous skin flap in 1-stage reconstruction of complex anterior urethral strictures. J Urol 1998;159:1209-13. [PubMed]
- Hudak SJ, Lubahn JD, Kulkarni S, et al. Single-stage reconstruction of complex anterior urethral strictures using overlapping dorsal and ventral buccal mucosal grafts. BJU Int 2012;110:592-6. [PubMed]
- Kulkarni S, Barbagli G, Sansalone S, et al. One-sided anterior urethroplasty: a new dorsal onlay graft technique. BJU Int 2009;104:1150-5. [PubMed]
- Palminteri E, Lazzeri M, Guazzoni G, et al. New 2-stage buccal mucosal graft urethroplasty. J Urol 2002;167:130-2. [PubMed]
- Andrich DE, Greenwell TJ, Mundy AR. The problems of penile urethroplasty with particular reference to 2-stage reconstructions. J Urol 2003;170:87-9. [PubMed]
- Burks FN, Santucci RA. Complicated urethroplasty: a guide for surgeons. Nat Rev Urol 2010;7:521-8. [PubMed]
- Barbagli G, De Angelis M, Palminteri E, et al. Failed hypospadias repair presenting in adults. Eur Urol 2006;49:887-94. [PubMed]
- Meeks JJ, Erickson BA, Gonzalez CM. Staged reconstruction of long segment urethral strictures in men with previous pediatric hypospadias repair. J Urol 2009;181:685-9. [PubMed]
- Mori R, Wood H, Angermeier K. Multistage buccal mucosa graft urethroplasty for complex anterior urethral strictures. J Urol 2014;191:e19-20.
- Kulkarni S, Barbagli G, Kirpekar D, et al. Lichen sclerosus of the male genitalia and urethra: surgical options and results in a multicenter international experience with 215 patients. Eur Urol 2009;55:945-54. [PubMed]
- Elliott SP, Eisenberg ML, McAninch JW. First-stage urethroplasty: utility in the modern era. Urology 2008;71:889-92. [PubMed]


