Advances in the treatment of testicular cancer
Despite their infrequency, accounting for only 1% of male malignancies in the United States, germ cell tumors (GCTs) have become an important oncological disease for several reasons. GCT is the most common malignancy in young men, 15-35 years old, and thus, has the potential to greatly shorten a man’s productive years. Second, GCT is amongst a unique group of neoplasms in whom biochemical markers play a critical role. In GCT’s serum tumor markers are an integral part of patient management as part of diagnosis, staging, risk assessment, evaluation of response to therapy and detection of relapse. Finally, GCT is a model of curable cancer, and a triumph of modern oncology. Current chemotherapy protocols and surgery yield cure rates exceeding 95% (1).
Epidemiology
GCTs affect young males with a median age at diagnosis of 34. The age-adjusted incidence rate in the United States is 5.6 per 100,000 men per year based on data from the Surveillance, Epidemiology and End Results (SEER) program between 2007 to 2011. The SEER database tracks incidence and survival data from specific geographic areas representing 26% of the U.S. population.
It is estimated that 8,820 new cases of testis cancer were diagnosed in the U.S. in 2007, while only 380 (4%) patients died of their disease. The lifetime risk of developing testis cancer is approximately 0.4% with an estimated 227,406 men living with testis cancer in the U.S. as of 2007. Improved survival over the last thirty years is attributed to the development of cisplatin combination chemotherapy. A high cure rate coupled with the young age at diagnosis has resulted in a growing population of testicular cancer survivors.
For unknown reasons, the incidence of GCT, particularly in Caucasian populations, is increasing globally. The lifetime risk of GCT’s in U.S. Caucasian men is estimated to be 1 in 230. In countries with the highest rate of GCTs, such as Demark, lifetime risk exceeds 1%. The SEER data indicates that between 1975 and 2004, the age-adjusted incidence rate of testicular cancer for males aged 15-49 years increased from 2.9 to 5.1 per 100,000 (2). This increase was more pronounced in seminoma compared to nonseminomatous germ cell tumor (NSGCT). The trend appears to be influenced by a birth cohort effect, where people born in a specific time interval show different risk compared to the period immediately preceding or following. For example, men born in Denmark and Norway during World War II have a lower risk of testicular cancer than either previous or subsequent birth cohorts (3).
Overall, rates of testicular cancer in industrialized nations are five times higher than those in less developed regions of the world. Further, considerable differences can be noted between neighboring countries and even within regions of the same country. For example, Denmark, Norway and Switzerland report age-standardized rates of roughly 9.5 per 100,000, while in Lithuania, Estonia, Spain and Latvia cancer incidence approaches 2 per 100,000 (4). Immigrant populations tend to carry the risk of their country of birth in the first generation, whereas, the risk of the second generation immigrants shifts toward the adopting population incidence (5). These observations coupled with the young age at presentation suggest an environmental risk factor acting in-utero or early in life. No specific etiological factors have yet been identified.
The incidence of testicular cancer varies with respect to race with the highest rate in Caucasian populations. The U.S. incidence among white men historically has been five times that of African American men (4). Recently, rates of testicular cancer for African American (6) and Hispanic young adults (7) living in the U.S. appear to be increasing. In contrast, Pacific Islanders, Asian, American Indian and Alaskan Natives have an intermediate risk. The native Maori of New Zealand are an exception with one of the highest incidence of testicular cancer in the world, exceeding even the local white European population (8).
Life expectancy of men beyond the second year post-diagnosis of testicular cancer is nearly identical to the general population (9); however, potential long-term risk exists for these patients. The contralateral testis may produce a second primary GCT in 2-5%. Late relapse of GCT affects approximately 3% of patients with NSGCT (10). Non-germ cell cancers are becoming an increasing problem following treatment of GCT. The 40-year cumulative incidence of a second malignant neoplasm may reach approximately one in three (11). In addition, survivors are at increased risk of developing delayed cardiovascular disease (12) as well as other treatment-related complications including neuropathy, nephro, oto, and pulmonary toxicity. Finally, sexual dysfunction and sub-fertility post treatment represent significant long-term morbidity in this young patient population (13).
Family history
The most consistent chromosomal anomaly in GCT is a gain of the short arm of chromosome 12—i(12p). Genetic syndromes linked to GCTs include Klinefelter syndrome which is associated with primary mediastinal GCT, and Down’s syndrome in which an increased rate of testicular seminoma is observed.
It is estimated that 1.4% of men with newly diagnosed GCT have a positive family history. This rate exceeds the degree expected by chance alone. Sons of men with testicular GCT have a four- to six-fold increased risk, while siblings of men with testicular GCT have an increased risk of eight- to ten-fold (14). The International Testicular Cancer Linkage Consortium is collaboration between multiple centers that holds the largest database of familial GCT published to date. A total of 985 patients from 461 families have been studied thus far. Clinical and pathologic characteristics were similar to those generally described for non-familial cases. However, an increased prevalence of testicular microlithiasis on sonography was found in men with familial testicular cancer and their relatives (15).
Unlike other hereditary cancers most GCT families consist of only two affected cases making genetic studies more difficult. Efforts are underway to find susceptibility genes for GCT within this unique group of familial cancers. Whether familial clusters of GCT are due to inherited mutations or simply reflect a shared environmental risk factor remains to be proven.
Therapeutic principles
In general, patients presenting with testicular cancer are divided into seminoma or nonseminomatous germ cell tumors (NSGCT). Management is based on volume of disease assessed using radiological staging and tumor marker level after orchiectomy. In low volume disease the goal is to decrease treatment related morbidity while maintaining a high cure rate. In patients presenting with advanced disease, especially those belonging to the intermediate and poor risk category, the goal of treatment is to improve response to chemotherapy with acceptable patient morbidity.
Seminoma
Seminoma represents approximately 60% of testicular GCTs. The incidence of testis tumors has risen over the last decade mostly due to seminomas (16). At presentation 80% of cases are stage I. Seminoma cases have a comparatively better prognosis than non-seminoma and stage III are very uncommon. Clinical research in GCT and seminoma in particular has led to a significant change in management. In the 1970’s and 1980’s treatment was based on radiation as this tumor is very radio-sensitive, however, the late effects of radiation and success of chemotherapy as curative treatment have changed the treatment algorithms. Currently, stage I patients are typically managed by surveillance alone, and stage II by a balance of radiation and chemotherapy.
Stage I
The main option is observation, where patients are followed by a careful schedule and treatment is opted for only in those who present with retroperitoneal or metastatic disease during follow-up (17). Outcome is excellent with almost 100% survival.
Radiation
Previously, radiation was given after diagnosis of stage I disease to prevent relapse. Most series published from single institutions reported very high survival rates and relapses were mainly outside of the radiation field—lungs, mediastinum and left supraclavicular fossa (18,19). The classical radiation fields followed areas of documented nodal involvement from surgical studies of modified retroperitoneal lymph node dissection (RPLND) templates, on the right in the peri-caval and interaorto caval areas down to the common iliac vessels, and on the left, periaortic from the renal vessels to the bifurcation of the common iliac. The lower border on both sides is placed at a level roughly mid pelvis covering the common iliac nodes yet sparing the bladder and prostate (20). The most important prospective studies in this setting showed that 20 Gy in 2 Gy daily fractions is ideal, though, carboplatin has an equivalent curing effect (21,22).
The main side effects of radiation are sterility, cardiovascular disease and second malignancies (12,23-25). Shielding of the contralateral testis has a protective effect and large studies have shown that modern radiation fields do not hamper sperm counts in the long run (26). A large National Cancer Institute (NCI) study documented the chance of second malignancies to be twice as high as healthy counterparts (27).
Surveillance
Surveillance of seminoma patients in stage I is now increasingly preformed. Disease relapse while on surveillance is seen in 15-20% (17,19,28), and is confined mainly to the retroperitoneum. Some groups tried to use a model based on high risk for relapse (primary testis tumor >4 cm and rete testis involvement) to direct management to radiation or carboplatin. Nonetheless, using this approach is not sufficiently accurate and 65% of patients may receive unnecessary treatment (29).
Most relapses appear in the first 2 to 3 years after diagnosis (30). As such, the tendency would be for close follow up early on to identify relapse early in its course. In the past this entailed a CT scan every 2 months in the first year and every 3 months in the second year; a not insignificant radiation exposure. As expected, such intense imaging has been scrutinized due to the potential danger of secondary malignancies. Most current guidelines recommend CT scanning every 6 months for the first 2 to 3 years. Despite the heightened attention to cumulative radiation exposure, diagnosis of relapse at an earlier stage with a smaller size of nodal disease allows for cure by radiation alone, whereas a higher disease load or relapse outside of the retroperitoneum necessitates use of chemotherapy.
Chemotherapy
Single agent carboplatin is the accepted alternative to radiation and surveillance (31). One or two cycles of carboplatin have reported relapse rates of 1.8-8.6% (17). The Medical Research Council (MRC) compared one cycle of carboplatin to adjuvant radiotherapy in nearly 1,500 patients. Updated results showed a 5-year relapse rate of 4% for radiotherapy and 5.3% for chemotherapy (32).
Management of relapse
Low volume retroperitoneal disease (i.e., less than 5 cm) may be cured by radiation. Large bulky disease or involvement of other organs is better treated by chemotherapy. Most cases may be cured by three courses of bleomycin, etoposide and cispatin (BEP) or four courses of EP. Rare cases of failure of primary chemo may be salvaged by local radiation or second line chemo therapy.
Stage II
Data accumulated in studies managing stage II seminoma show that for tumor size up to 5 cm radiation is an acceptable treatment modality with a 5-year relapse rate of up to 9%. Bulkier disease is best treated by chemotherapy with relapse rates of 6-13.5% (33-36). Recent studies as in SWENOTECA have shown the superiority of chemotherapy also in lower stages—seminoma IIa/b (37). The primary consideration for choice of therapy is chemotoxicity in older age patients where radiation may have fewer side effects. Radiation fields in this setting are similar to stage I, limiting pelvic radiation to the level of the acetabulum.
A residual mass after radiation or chemotherapy is a unique challenge. In contrast to NSGCT post-chemotherapy residual disease where teratoma or cancer may be frequently found, most residual seminoma masses harbor fibrosis or necrosis. PET-CT may reliably indicate the presence of active tumor; therefore a negative PET-CT may allow observation even in large redial masses. Some centers advocate resection of all masses larger than 3 cm (38), though, this may be a difficult undertaking due to the desmoplastic reaction and adherence to the main blood vessels.
NSGCT
Clinical stage I (CSI)
Clinical stage I accounts for 50-60% of non-seminomatous testicular tumors. It is long known that the risk of occult metastatic disease (not identified on imaging) is dependent on the presence of lymphovascular invasion (LVI) in the tumor (39-41). LVI is present in about 30% of cases and the risk of recurrence is about 50% with LVI versus 15-20% without LVI (42,43). Another less accepted risk factor is embryonal predominance, with controversial data among different studies (41-43). Recurrences occur most commonly in the retroperitoneum, with the majority diagnosed within 2 years of orchiectomy (42,44). Management options for CSI NSGCT include surveillance, RPLND, and adjuvant chemotherapy.
Surveillance
The rationale for surveillance among patients with CSI NSGCT is that studies have shown that approximately one in four patients will recur and require salvage treatment (39-41). This is the group that actually would benefit from adjuvant therapy, whereas most patients will not benefit. Active surveillance became an option in the 1980’s when Read et al. demonstrated that cisplatin-based chemotherapy could cure almost all recurrences (45). When studies revealed the importance of LVI as a prognostic factor for recurrence, risk-adapted approaches with surveillance or adjuvant treatment were implemented (46,47). At present, some centers advocate surveillance for all CSI NSGCT, consequently no patient will be treated unnecessarily; however, 50% of those with LVI and 15% of the patients without LVI will later need salvage treatment (41,46,47).
RPLND
Although not frequently used today, the advantage of RPLND is that it represents both a diagnostic and a therapeutic procedure. RPLND remains the most accurate means of staging patients with CSI NSGCT; roughly 50% to 70% will be pathologic stage I. In these patients, RPLND is purely diagnostic with the added benefit of a simpler follow up. Because retroperitoneal recurrence is rare with properly performed RPLND, abdominal CT scan may be omitted after negative RPLND. In the case of pathologic stage II disease RPLND is curative in 50% to 90% of patients, thus selected patients may avoid adjuvant chemotherapy (24,48).
Adjuvant chemotherapy
As noted previously, 50% of LVI positive patients will relapse, therefore adjuvant treatment would spare half of this group from a recurrence requiring three to four courses of chemotherapy and possibly post-chemotherapy surgery (PCS) for a residual tumor. Conversely, the other half would receive adjuvant chemotherapy ‘unnecessarily’. The main argument against adjuvant chemotherapy is its lack of improved overall survival and its association with long-term side effects including infertility, secondary malignancies, and increased risk for cardiovascular disease, impaired kidney function, hearing impairment, and peripheral neuropathy (48-50).
One way to reduce toxicity of adjuvant chemotherapy is to reduce the number of cycles used (51,52). The German testicular study group published data in 2008 from a randomized study on 382 patients with CSI NSGCT. Patients were randomized to RPLND (in the community) or BEP ×1 without regard to LVI. This was a non-inferiority study with a median follow-up of 4.7 years and a primary endpoint of recurrence rate. The recurrence rate was 1% and 7.9% for patients treated with BEP ×1 and RPLND, respectively. About 40% of each group were LVI-positive (53). The main criticism of this study is that RPLND was performed in less skilled hands as evidenced by unacceptably high in-field recurrence rates.
SWENOTECA—the Swedish-Norwegian testicular cancer group now comprises all centers treating testicular cancer patients in Sweden and Norway. Based on the results from earlier treatment protocols a new risk-adapted treatment protocol for CSI NSGCT was initiated in 1995.
During the period of 1995-1997, 232 patients were accrued to the SWENOTECA III protocol. CSI NSGCT LVI- patients were randomized to cisplatin, vinblastin, bleomycin (CVB) ×1, or surveillance. LVI+ patients were treated with CVB ×2 and data was collected prospectively. The recurrence rate among the CVB ×1 patients was higher than expected and as such, the study was terminated early (54).
SWENOTECA VI randomized low-risk patients (LVI-) to surveillance or BEP ×1, and high-risk patients (LVI+) to BEP ×2 or BEP ×1. Yearly assessments of the total cohort were performed and low relapse rates with BEP ×1 were noted. Accordingly, the protocol was amended to treat high-risk patients with BEP ×1. In 2009 results with a median follow-up of 4.7 years were reported. A total of 313 patients were treated with one course of adjuvant BEP (157 LVI+, 155 LVI– and 1 LVI unknown). The relapse rate was 3.2% for LVI+ and 1.3% for LVI– (47).
Recently, the expanded data from a total of 517 patients (258 LVI+, 255 LVI– and 4 LVI unknown) treated with one course of adjuvant BEP between 1998 and 2010 was reported (44). The median follow-up was 7.9 years. The data confirmed the SWENOTECAs earlier reported low relapse rates as well as excellent overall- and cause-specific survival. Only one patient died because of progressive cancer and there were no treatment related deaths. Five of the 12 relapses (42%) were cured by RPLND alone, and only 1.4% (7/517) of the patients actually required salvage chemotherapy. These findings confirm that one course of adjuvant BEP reduces the risk of relapse by 90-95% in all patients. No recurrences occurred later than 3.3 years post-treatment and as such, follow-up can safely be reduced to 5 years (55).
The optimal treatment strategy for CSI NSGCT is controversial. To date, there are no randomized trials that demonstrate superiority of surveillance or adjuvant treatment. Further, cure approaches 100% regardless of treatment strategy. Thus the main issue is how to best minimize treatment related toxicity. As noted earlier, chemotherapy increases the risks of cardiovascular damage resulting in hypertension, cardiac events, and decreased kidney function. Impaired hearing, metabolic late effects, hypogonadism and increased risk for secondary cancers are also associated with adjuvant chemotherapy. As well, there is a clear dose-response relationship associated with increased cycles of chemotherapy. For stage I NSGCT, results from the SWENOTECA study show that adjuvant therapy can be safely reduced to just one course of BEP, resulting in a reduction in relapse rate of 90-95%. This lower dose of chemotherapy may mitigate many of the long-term consequences of therapy.
Clinical stage II (CSII) and III (CSIII)
In metastatic NSGCT, the degree of marker elevation before chemotherapy correlates with prognosis. The International Germ Cell Cancer Collaborative Group (IGCCCG) has incorporated serum concentrations of human chorionic gonadotrophin (hCG), AFP, and lactic dehydrogenase (LDH) into a prognostic classification system with high, intermediate, and low risk disease (Table 1), and treatment is tailored according to the risk assignment. Systemic therapy for metastatic GCT consists of cisplatin-based chemotherapy. For good risk disease, the accepted standard is three courses of BEP or four courses of EP. Standard therapy for intermediate and poor risk disease remains four courses of BEP.
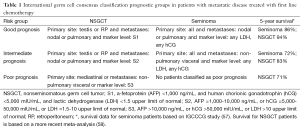
Full table
Depending upon the patient population selected, roughly 70% of patients treated with first line chemotherapy will have complete radiographic and biochemical response. In the remaining 30% a residual mass will persist after chemotherapy, most commonly in the retroperitoneum (58,59). These patients will then undergo post-chemotherapy retroperitoneal lymph node dissection (PC-RPLND) because of possible residual teratoma (40%) or active cancer (10%) (60).
Controversies in PC-RPLND
The excision of all masses after chemotherapy, within and outside the boundaries of the retroperitoneum, is integral to the cure of NSGCT (61). It is well recognized that incomplete resection or surveillance of a residual mass after chemotherapy risks relapse (62,63). Therefore, any patient who has a mass larger than 1 cm in the retroperitoneum should undergo surgery. The proper extent of PCS resection and the need for PC-RPLND in patients achieving complete remission remains controversial (64,65).
At most centers, the management of patients achieving a complete radiographic response to systemic chemotherapy is observation. However, studies have documented the incidence of residual teratoma in sub-centimeter retroperitoneal nodes following chemotherapy to be 20-30% (66-68). Therefore, some institutions have adopted a policy of PC-RPLND in all patients, including those achieving complete radiographic response.
A study from Indiana University analyzed 141 consecutive patients who achieved complete remission following first-line induction chemotherapy (64). All patients were observed and did not undergo immediate PC-RPLND. Patients who had intermediate or poor prognosis disease constituted 23% of the cohort. After a median follow-up of 15.5 years, 12 patients experienced a relapse, of who four died of their disease. Amongst these four, the relapse occurred within the first year of chemotherapy; in two of them, the retroperitoneum was the site of relapse. Altogether, of the 141 patients, six (4%) relapses occurred in the retroperitoneum. The estimated 15-year cancer-specific survival rate was 97%.
The data suggest that patients that relapse in the retroperitoneum on observation (4%) remain curable. It is unlikely that a different strategy could result in a higher 15 years cancer-specific survival. In other words, there is no evidence that immediate PC-RPLND would prevent those rare relapses in exchange for subjecting all patients to the morbidity of PC-RPLND. Two other North American studies similarly support the safety of observation (69,70). The current European and Canadian guidelines endorse this data and favor observation for patients achieving complete radiographic remission, whereas in the NCCN guidelines either immediate PC-RPLND or observation are appropriate.
The second area of controversy is the extent of PC-RPLND. The extent of primary RPLND for stage I NSGCT has changed considerably over the last three decades from a full bilateral suprahilar dissection to a unilateral nerve sparring template without compromising cure. Unlike primary RPLND, in the management of post-chemotherapy retroperitoneal disease there has been no such reduction in surgical boundaries with full bilateral dissection considered standard therapy.
In the 1970’s and 1980’s lower stage metastatic disease was more often treated with primary bilateral template RPLND in an attempt to avoid chemotherapy which had considerable morbidity at the time. With the improvement of antiemetic, growth factors and supportive care, the toxicity of chemotherapy has decreased. Today only select patients with limited retroperitoneal disease who have normalized serum tumor markers may be considered for primary RPLND (71). Patients with teratoma or non-germ cell component in their primary tumor can benefit the most from primary RPLND (72).
Based on early experience from primary RPLND, retroperitoneal mapping studies have accurately documented the lymphatic spread of metastasis (73,74). Metastases right of the vena cava were rare in patients with a left-sided primary (3-7%), but crossover metastases left of the aorta were more common in patients with a right sided primary (8-19%). Theoretically, had chemotherapy been administered before surgery, it would not have changed the retroperitoneal distribution of the residual tumors, suggesting that template crossover after chemotherapy is not generally expected in low-stage left-sided tumors. Our group has shown from our experience with bilateral PC-RPLND that patients with left-sided primary tumors and clinical stage IIA or IIB disease at presentation did not have metastasis right of the aorta (75). In these patients it may be safe to perform a left modified dissection. Beck et al. (76) and Heidenreich et al. (77) have further shown that a modified unilateral PC-RPLND (either right or left) may be safe in select patients with low volume retroperitoneal disease (less than 5 cm), restricted to the primary landing zone of the affected testicle.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Einhorn LH. Curing metastatic testicular cancer. Proc Natl Acad Sci U S A 2002;99:4592-5. [PubMed]
- Holmes L Jr, Escalante C, Garrison O, et al. Testicular cancer incidence trends in the USA (1975-2004): plateau or shifting racial paradigm? Public Health 2008;122:862-72. [PubMed]
- Bergström R, Adami HO, Möhner M, et al. Increase in testicular cancer incidence in six European countries: a birth cohort phenomenon. J Natl Cancer Inst 1996;88:727-33. [PubMed]
- Znaor A, Lortet-Tieulent J, Jemal A, et al. International variations and trends in testicular cancer incidence and mortality. Eur Urol 2014;65:1095-106. [PubMed]
- Schmiedel S, Schüz J, Skakkebaek NE, et al. Testicular germ cell cancer incidence in an immigration perspective, Denmark, 1978 to 2003. J Urol 2010;183:1378-82. [PubMed]
- McGlynn KA, Devesa SS, Graubard BI, et al. Increasing incidence of testicular germ cell tumors among black men in the United States. J Clin Oncol 2005;23:5757-61. [PubMed]
- Chien FL, Schwartz SM, Johnson RH. Increase in testicular germ cell tumor incidence among Hispanic adolescents and young adults in the United States. Cancer 2014;120:2728-34. [PubMed]
- Sarfati D, Shaw C, Blakely T, et al. Ethnic and socioeconomic trends in testicular cancer incidence in New Zealand. Int J Cancer 2011;128:1683-91. [PubMed]
- Capocaccia R, Gatta G, Dal Maso L. Life expectancy of colon, breast, and testicular cancer patients: an analysis of US-SEER population-based data. Ann Oncol 2015;26:1263-8. [PubMed]
- Baniel J, Foster RS, Gonin R, et al. Late relapse of testicular cancer. J Clin Oncol 1995;13:1170-6. [PubMed]
- Travis LB, Fosså SD, Schonfeld SJ, et al. Second cancers among 40,576 testicular cancer patients: focus on long-term survivors. J Natl Cancer Inst 2005;97:1354-65. [PubMed]
- Haugnes HS, Wethal T, Aass N, et al. Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study. J Clin Oncol 2010;28:4649-57. [PubMed]
- Travis LB, Beard C, Allan JM, et al. Testicular cancer survivorship: research strategies and recommendations. J Natl Cancer Inst 2010;102:1114-30. [PubMed]
- Greene MH, Kratz CP, Mai PL, et al. Familial testicular germ cell tumors in adults: 2010 summary of genetic risk factors and clinical phenotype. Endocr Relat Cancer 2010;17:R109-21. [PubMed]
- Korde LA, Premkumar A, Mueller C, et al. Increased prevalence of testicular microlithiasis in men with familial testicular cancer and their relatives. Br J Cancer 2008;99:1748-53. [PubMed]
- Shah MN, Devesa SS, Zhu K, et al. Trends in testicular germ cell tumours by ethnic group in the United States. Int J Androl 2007;30:206-13; discussion 213-4. [PubMed]
- Chung P, Mayhew LA, Warde P, et al. Management of stage I seminomatous testicular cancer: a systematic review. Clin Oncol (R Coll Radiol) 2010;22:6-16. [PubMed]
- Chung P, Warde P. Testicular cancer: seminoma. BMJ Clin Evid 2011;2011.
- Kamba T, Kamopto T, Okubo K, et al. Outcome of different post-orchiectomy management for stage I seminoma: Japanese multi-institutional study including 425 patients. Int J Urol 2010;17:980-7. [PubMed]
- Classen J, Schmidberger H, Meisner C, et al. Para-aortic irradiation for stage I testicular seminoma: results of a prospective study in 675 patients. A trial of the German testicular cancer study group (GTCSG). Br J Cancer 2004;90:2305-11. [PubMed]
- Mead GM, Fossa S, Oliver T, et al. Randomized trials in 2466 patients with stage I seminoma: patterns of relapse and follow-up. J Natl Cancer Inst 2011;103:241-9. [PubMed]
- Jones WG, Fossa S, Mead G, et al. Randomized trial of 30 vs. 20 Gy in the adjuvant treatment of stage I seminoma. A report on MRC trial TE18, EORTC 20942. J Clin Oncol 2005;23:1200-8. [PubMed]
- Jacobsen KD, Olsen D, Fossa K, et al. External beam abdominal radiotherapy in patients with seminoma stage I: field type, testicular dose and spermatogenesis. Int J Radiat Oncol Biol Phys 1997;38:95-102. [PubMed]
- Huddart RA, Norman A, Shahidi M, et al. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J Clin Oncol 2003;21:1513-23. [PubMed]
- Zagars GK, Ballo MT, Lee AK, et al. Mortality after cure of testicular seminoma. J Clin Oncol 2004;22:640-7. [PubMed]
- Fosså SD, Horwich A, Russell JM, et al. Optimal planning target volume for stage I testicular seminoma: A Medical Research Council randomized trial. Medical Research Council Testicular Tumor Working Group. J Clin Oncol 1999;17:1146. [PubMed]
- Beard CJ, Travis LB, Chen MH, et al. Outcomes in stage I testicular seminoma: a population based study of 9193 patients. Cancer 2013;119:2771-7. [PubMed]
- Yoshida T, Kakimoto K, Takezawa K, et al. Surveillance following orchiectomy for seminoma stage I: long term outcome. Int J Urol 2009;16:756-9. [PubMed]
- Cummins S, Yau T, Huddart R, et al. Surveillance in stage I seminoma patients: a long-term assessment. Eur Urol 2010;57:673-8. [PubMed]
- Martin JM, Panzarella T, Zwahlen DR, et al. Evidence-based guidelines for following stage 1 seminoma. Cancer 2007;109:2248-56. [PubMed]
- Beyer J, Albers P, Altena R, et al. Maintaining success, reducing treatment burden, focusing on survivorship highlights from the third European consensus conference on diagnosis and treatment of germ cell cancer. Ann Oncol 2013;24:878-88. [PubMed]
- Oliver RT, Mead GM, Rustin GJ, et al. Randomized trial of carboplatin versus radiotherapy for stage I seminoma: mature results on relapse and contralateral testis cancer rates in MRC TE19/EORTC 30982 study (ISRCTN27163214). J Clin Oncol 2011;29:957-62. [PubMed]
- Chung PW, Gospodarowicz MK, Panzarella T, et al. Stage II testicular seminoma: patterns of recurrence and outcome of treatment. Eur Urol 2004;45:754-59; discussion 759-60. [PubMed]
- Classen J, Schmidberger H, Meisner C, et al. Radiothrapy for classes IIA/B testicular seminoma. J Clin Oncol 2003;21:1101-6. [PubMed]
- Vallis KA, Howard GC, Duncan W, et al. Radiotherapy for stages I and II testicular seminoma: results and morbidity in 238 patients. Br J Radiol 1995;68:400-5. [PubMed]
- Zagars GK, Pollack A. Radiotherapy for stage II testicular seminoma. Int J Radiat Oncol Biol Phys 2001;51:643-9. [PubMed]
- Tandstad T, Smaaland R, Solberg A, et al. Management of seminomatous testicular cancer: a binational prospective population-based study from the Swedish norwegian testicular cancer study group. J Clin Oncol 2011;29:719-25. [PubMed]
- Herr HW, Sheinfeld J, Puc HS, et al. Surgery for a postchemotherapy residual mass in seminoma. J Urol 1997;157:860-2. [PubMed]
- Klepp O, Olsson AM, Ous S, et al. Early clinical stages of nonseminomatous testis cancer. Evaluation of the primary treatment and follow-up procedures of the SWENOTECA project. Scand J Urol Nephrol 1991;25:179-90. [PubMed]
- Pont J, Albrecht W, Postner G, et al. Adjuvant chemotherapy for high-risk clinical stage I nonseminomatous testicular germ cell cancer: long-term results of a prospective trial. J Clin Oncol 1996;14:441-8. [PubMed]
- Albers P, Siener R, Kliesch S, et al. Risk factors for relapse in clinical stage I nonseminomatous testicular germ cell tumors: results of the German Testicular Cancer Study Group Trial. J Clin Oncol 2003;21:1505-12. [PubMed]
- Kollmannsberger C, Moore C, Chi KN, et al. Non-risk-adapted surveillance for patients with stage I nonseminomatous testicular germ-cell tumors: diminishing treatment-related morbidity while maintaining efficacy. Ann Oncol 2010;21:1296-301. [PubMed]
- Sturgeon JF, Moore MJ, Kakiashvili DM, et al. Non-risk-adapted surveillance in clinical stage I nonseminomatous germ cell tumors: the Princess Margaret Hospital's experience. Eur Urol 2011;59:556-62. [PubMed]
- Tandstad T, Ståhl O, Håkansson U, et al. One course of adjuvant BEP in clinical stage I nonseminoma mature and expanded results from the SWENOTECA group. Ann Oncol 2014;25:2167-72. [PubMed]
- Read G, Stenning SP, Cullen MH, et al. Medical Research Council prospective study of surveillance for stage I testicular teratoma. Medical Research Council Testicular Tumors Working Party. J Clin Oncol 1992;10:1762-8. [PubMed]
- Studer UE, Burkhard FC, Sonntag RW. Risk adapted management with adjuvant chemotherapy in patients with high risk clinical stage i nonseminomatous germ cell tumor. J Urol 2000;163:1785-7. [PubMed]
- Tandstad T, Dahl O, Cohn-Cedermark G, et al. Risk-adapted treatment in clinical stage I nonseminomatous germ cell testicular cancer: the SWENOTECA management program. J Clin Oncol 2010;28:1438. [PubMed]
- Meinardi MT, Gietema JA, van der Graaf WT, et al. Cardiovascular morbidity in long-term survivors of metastatic testicular cancer. J Clin Oncol 2000;18:1725-32. [PubMed]
- Nord C, Bjoro T, Ellingsen D, et al. Gonadal hormones in long-term survivors 10 years after treatment for unilateral testicular cancer. Eur Urol 2003;44:322-8. [PubMed]
- Haugnes HS, Bosl GJ, Boer H, et al. Long-term and late effects of germ cell testicular cancer treatment and implications for follow-up. J Clin Oncol 2012;30:3752-63. [PubMed]
- Gilbert DC, Norman AR, Nicholl J, et al. Treating stage I nonseminomatous germ cell tumours with a single cycle of chemotherapy. BJU Int 2006;98:67-9. [PubMed]
- Westermann DH, Schefer H, Thalmann GN, et al. Long-term followup results of 1 cycle of adjuvant bleomycin, etoposide and cisplatin chemotherapy for high risk clinical stage I nonseminomatous germ cell tumors of the testis. J Urol 2008;179:163-6. [PubMed]
- Albers P, Siener R, Krege S, et al. Randomized phase III trial comparing retroperitoneal lymph node dissection with one course of bleomycin and etoposide plus cisplatin chemotherapy in the adjuvant treatment of clinical stage I Nonseminomatous testicular germ cell tumors: AUO trial AH 01/94 by the German Testicular Cancer Study Group. J Clin Oncol 2010;28:1439. [PubMed]
- Tandstad T, Cohn-Cedermark G, Dahl O, et al. Long-term follow-up after risk-adapted treatment in clinical stage 1 (CS1) nonseminomatous germ-cell testicular cancer (NSGCT) implementing adjuvant CVB chemotherapy. A SWENOTECA study. Ann Oncol 2010;21:1858-63. [PubMed]
- Kollmannsberger C, Tandstad T, Bedard PL, et al. Patterns of relapse in patients with clinical stage I testicular cancer managed with active surveillance. J Clin Oncol 2015;33:51-7. [PubMed]
- International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J Clin Oncol 1997;15:594-603. [PubMed]
- van Dijk MR, Steyerberg EW, Habbema JD. Survival of non-seminomatous germ cell cancer patients according to the IGCC classification: An update based on meta-analysis. Eur J Cancer 2006;42:820-6. [PubMed]
- Einhorn LH, Williams SD, Loehrer PJ, et al. Evaluation of optimal duration of chemotherapy in favorable-prognosis disseminated germ cell tumors: a Southeastern Cancer Study Group protocol. J Clin Oncol 1989;7:387-91. [PubMed]
- de Wit R, Stoter G, Kaye SB, et al. Importance of bleomycin in combination chemotherapy for good-prognosis testicular nonseminoma: a randomized study of the European Organization for Research and Treatment of Cancer Genitourinary Tract Cancer Cooperative Group. J Clin Oncol 1997;15:1837-43. [PubMed]
- Vergouwe Y, Steyerberg EW, Foster RS, et al. Predicting retroperitoneal histology in postchemotherapy testicular germ cell cancer: a model update and multicentre validation with more than 1000 patients. Eur Urol 2007;51:424-32. [PubMed]
- Sonneveld DJ, Sleijfer DT, Koops HS, et al. Mature teratoma identified after postchemotherapy surgery in patients with disseminated nonseminomatous testicular germ cell tumors: a plea for an aggressive surgical approach. Cancer 1998;82:1343-51. [PubMed]
- Hendry WF, Norman AR, Dearnaley DP, et al. Metastatic nonseminomatous germ cell tumors of the testis: results of elective and salvage surgery for patients with residual retroperitoneal masses. Cancer 2002;94:1668-76. [PubMed]
- Debono DJ, Heilman DK, Einhorn LH, et al. Decision analysis for avoiding postchemotherapy surgery in patients with disseminated nonseminomatous germ cell tumors. J Clin Oncol 1997;15:1455-64. [PubMed]
- Ehrlich Y, Brames MJ, Beck SD, et al. Long-term follow-up of Cisplatin combination chemotherapy in patients with disseminated nonseminomatous germ cell tumors: is a postchemotherapy retroperitoneal lymph node dissection needed after complete remission? J Clin Oncol 2010;28:531-6. [PubMed]
- Bosl GJ, Motzer RJ. Weighing risks and benefits of postchemotherapy retroperitoneal lymph node dissection: not so easy. J Clin Oncol 2010;28:519-21. [PubMed]
- Oldenburg J, Alfsen GC, Lien HH, et al. Postchemotherapy retroperitoneal surgery remains necessary in patients with nonseminomatous testicular cancer and minimal residual tumor masses. J Clin Oncol 2003;21:3310-7. [PubMed]
- Karellas M, Carver BS, Stasi J, et al. Clinical outcome following post-chemotherapy retroperitoneal lymph node dissection for men with CII non-seminomatous germ cell tumors and a radiographically normal retroperitoneum. J Urol 2007;177:277, abstr 830.
- Steiner H, Akkad T, Gozzi C, et al. High rate of retroperitoneal teratoma despite complete remission after chemotherapy for metastatic nonseminomatous germ cell tumor. J Urol 2007;177:277, abstr 831.
- Kollmannsberger C, Daneshmand S, So A, et al. Management of disseminated nonseminomatous germ cell tumors with risk-based chemotherapy followed by response-guided postchemotherapy surgery. J Clin Oncol 2010;28:537-42. [PubMed]
- Ravi P, Gray KP, O'Donnell EK, et al. A meta-analysis of patient outcomes with subcentimeter disease after chemotherapy for metastatic non-seminomatous germ cell tumor. Ann Oncol 2014;25:331-8. [PubMed]
- Stephenson AJ, Bosl GJ, Motzer RJ, et al. Nonrandomized comparison of primary chemotherapy and retroperitoneal lymph node dissection for clinical stage IIA and IIB nonseminomatous germ cell testicular cancer. J Clin Oncol 2007;25:5597-602. [PubMed]
- Ehrlich Y, Beck SD, Ulbright TM, et al. Outcome analysis of patients with transformed teratoma to primitive neuroectodermal tumor. Ann Oncol 2010;21:1846-50. [PubMed]
- Donohue JP, Zachary JM, Maynard BR. Distribution of nodal metastases in nonseminomatous testis cancer. J Urol 1982;128:315-20. [PubMed]
- Weissbach L, Boedefeld EA. Localization of solitary and multiple metastases in stage II nonseminomatous testis tumor as basis for a modified staging lymph node dissection in stage I. J Urol 1987;138:77-82. [PubMed]
- Ehrlich Y, Yossepowitch O, Kedar D, et al. Distribution of nodal metastases after chemotherapy in nonseminomatous testis cancer: a possible indication for limited dissection. BJU Int 2006;97:1221-4. [PubMed]
- Beck SD, Foster RS, Bihrle R, et al. Is full bilateral retroperitoneal lymph node dissection always necessary for postchemotherapy residual tumor? Cancer 2007;110:1235-40. [PubMed]
- Heidenreich A, Pfister D, Witthuhn R, et al. Postchemotherapy retroperitoneal lymph node dissection in advanced testicular cancer: radical or modified template resection. Eur Urol 2009;55:217-24. [PubMed]


