The enigma of men with interstitial cystitis/bladder pain syndrome
Introduction
Interstitial cystitis/bladder pain syndrome (IC/BPS) is most often characterized as an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptom(s) of more than 6 weeks duration, in the absence of infection or other identifiable causes (1). Often the discomfort felt worsens with bladder filling and improves with bladder emptying (2). It has traditionally been considered a disease of women and until recently, very few published papers have focused on the condition in men.
The number of diagnoses of interstitial cystitis (IC) has continued to grow over the past 40 years. Early estimates in the United States projected 10 cases per 100,000 people in 1975 with a female to male predominance of 10:1 (3). Modern studies support a much higher prevalence of IC—up to 197 cases per 100,000 women and 41 cases per 100,000 men in 2005. A more recent study suggests that the prevalence in men may be higher than previously thought, closer to 20% of the total number of afflicted individuals (4). However this latter study used diagnosis codes (ICD-9 code 595.1) to determine the prevalence of IC in a regional health maintenance organization (HMO), and so may only represent patients who both sought medical care for their symptoms and were subsequently assigned a diagnosis by a provider, which suggests that the true prevalence of IC/BPS may be higher. It has been suggested that this rise in prevalence may be due to an under-diagnosis and misdiagnosis of IC/BPS in men (5).
Often the diagnosis of IC/BPS is delayed in both genders. Men in particular are often misdiagnosed early on as prostatitis, benign prostatic enlargement, or epididymitis and are shuffled through a variety of providers before a diagnosis of IC/BPS is made. Sexual dysfunction is present in as common as 71% of men with IC/BPS (6). Like chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), IC if often associated with similar rates of psychosocial depression (5).
Men provide unique challenges to practitioners both in the diagnosis and treatment of IC/BPS, and very few studies to date have included substantive numbers of male patients or have taken into consideration the challenges that male patients present.
Misdiagnosis and overlap with CP/CPPS
IC/BPS is often grouped with another chronic pain disorder in men: CP/CPPS. Prostatitis was the initial diagnosis in almost half of men with IC/BPS in one early study, followed closely by benign prostatic hyperplasia (BPH) (7). Both IC/BPS and CP/CPPS are not simply diseases with one identifiable cause but instead are syndromes, so understandably there has been a lot of confusion in diagnosis and treatment. Some have suggested that there exists overlap in the pathophysiology of the two syndromes, however a key difference is the presence of bladder pathology often seen in IC/BPS (8). CP/CPPS is described as chronic (often >3 months duration) genitourinary pain in the absence of uropathogenic bacteria, localized to the prostate gland employing standard methodology in the absence of an identifiable inflammatory component (9,10). Prostatitis is consistently the most common initial diagnosis in men who are ultimately found to have IC/BPS (8,11,12). The key symptom defining IC/BPS in both the American Urological Association (AUA) and International Society for the Study of Bladder Pain Syndrome (ESSIC) guidelines are symptoms “perceived to be related to the urinary bladder”. Since men have a prostate and women do not, this perception related to pelvic pain is more likely to be made to the bladder in women and prostate in men. It is important to consider both diagnoses when approaching men with chronic pelvic pain of undetermined origin in order to begin the most appropriate treatment early so as to avoid delay and further progression of the process, particularly when standard treatment approaches for either syndrome are not working.
One of the earlier studies to suggest a common misdiagnosis of prostatitis was by Berger and colleagues, in which 60 patients at the University of Washington clinic with a diagnosis of prostate pain in the absence of bacteriuria underwent cystoscopy and hydrodistension under anesthesia. Using the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) criteria for IC, the authors looked for the presence of petechiae on the bladder mucosa, which they graded according to extent and severity of appearance. Of these, 58% were classified as “moderate/severe”. This group was found to have fewer leukocytes within expressed prostatic secretions, smaller bladder volumes, and less testicular pain than the group with milder findings. Interestingly, this group also was more likely to note improvement in symptoms after the initial hydrodistension (12). While the presence glomerulations has now been dropped as a diagnostic criterion due to its non-specificity, this was the first systematic study to suggest a higher proportion of CP/CPPS men actually having IC.
Few studies have compared the two syndromes directly. One such investigation, the RAND Interstitial Cystitis Epidemiology (RICE) male study, was conducted as a national population-based screening program in response to a state’s need for more comprehensive research on the problem of IC/BPS in men. The study authors utilized a previously developed questionnaire for chronic pelvic pain syndrome (CPPS) validated in a male population, and a previously developed questionnaire for IC/BPS validated in a female population and applied both to men (with some adjustments to the latter to exclude female-specific modifiers such as pregnancy and gynecological cancers). Two different definitions of IC/BPS were used, one with a high (81%) sensitivity and another with a high (83%) specificity for IC/BPS. Exclusion criteria were similar to the NIDDK definition. Of the 149 men surveyed, 1.9-4.2% were positive for IC/BPS while 1.8% were positive for CPPS. The same IC/BPS questionnaire used in women found a prevalence of 2.70-6.53% (13). The estimates from this study are higher than the epidemiological approach taken by the Boston Area Community Health Survey of over 5,500 individuals age 30-79 years old in the Boston area, which found a prevalence of IC/BPS of 1.3% in men and 2.6% in women (14). Interestingly, the RICE study found a 17% overlap between respondents who were positive for both IC/BPS and CPPS. Prior studies have not shown comparative overlaps between the two syndromes, and the authors suggest that this provides evidence for a possible common pathophysiological origin. Furthermore it is noted that a diagnosis of either condition in men warrants consideration or at least an elevated index of suspicion for the other diagnosis, particularly as the provider considers potential treatment options (15,16).
Diagnosis
The diagnostic criteria of the syndrome itself has gone through many changes over the past few decades (17). Initial diagnosis is often made based on a patient-reported history of discomfort in the pelvic region associated with bladder filling that is relieved with voiding (2). This discomfort often manifests itself as pressure, pain, or bladder spasms and can range from very mild to severe and debilitating, often becoming very disruptive to a patient’s home and work life due to the chronic pain as well as associated urinary frequency (18). Specific diagnostic criteria are lacking, definitive histopathological changes are inconsistent, and symptoms fluctuate unpredictably. Moreover the variability between patients’ symptoms, physical findings, and responses to treatment are tremendous (19). The general theme of IC/BPS is that of a prolonged syndrome of pain localized to the pelvis, associated with irritative voiding symptoms (usually urinary frequency) that cannot be explained by any other pathological processes. A key point distinguishing the urinary frequency of BPH and IC/BPS is that an IC/BPS patient will say he voids frequently to reduce pain rather than due to the typical urgency seen with BPH patients.
A set of consensus criteria developed by the NIDDK was agreed upon for the diagnosis of IC with the intention that researchers between institutions would have comparable patient populations. These were not intended to be used as a diagnostic algorithm for clinicians, but in the absence of a suitable clear alternative these had become the generally accepted criteria used for a new diagnosis of IC/BPS (20). In a 1998 review of the NIDDK Interstitial Cystitis Data Base (ICDB) by Hanno and colleagues of 379 patients with a diagnosis of IC, the authors found that only 31.1% strictly met the NIDDK criteria. Of the patients who did not meet all NIDDK criteria, it was found that of this group 86.6% were classified as having a very likely/definite diagnosis of IC. The authors determined that strict application of the NIDDK criteria would miss up to 60% of patients who might otherwise be identified as suffering from IC (21). It should be noted that this study was of women only, and excluded men due to a concern that there would be potentially confounding diagnoses.
History and physical exam
The key elements of a history of IC/BPS in men include the presence of urinary frequency or urgency and pain that worsens as the bladder fills and improves or resolves, at least temporarily, when the bladder empties (5). In addition, men will often have suprapubic tenderness on examination. Tenderness of the prostate typically points to CP/CPPS as the primary diagnosis, however an inexperienced examiner may often report anterior pelvic floor spasm as prostatic tenderness.
Laboratory findings
Unfortunately there are no universally accepted laboratory tests that consistently confirm a diagnosis of IC/BPS. Diagnostic workup includes a urinalysis with microscopic examination, which may reveal hematuria in 33-40% of patients, a factor that is not considered a major component in CP/CPPS (8). Urine culture is also indicated to rule out infection.
No definitive biomarkers have been discovered that can be used with clinically applicable reliable sensitivity and specificity for IC/BPS. Like CP/CPPS, IC/BPS is a syndrome—a complex of symptoms that is not otherwise explained by any other pathophysiological process. The use of laboratory tests can be used to rule out other conditions such as chronic bacterial prostatitis or urinary tract infection, but at this time the ability to confirm a diagnosis using makers in urine, blood, or other body sera is not yet validated and not part of any published guidelines (19).
One of the most promising biomarkers has been the presence of antiproliferative factor (APF) in urine. In a 2004 study by Keay and colleagues, 101 men with CP/CPPS, IC or asymptomatic controls were evaluated for urinary levels of APF, heparin-binding epidermal growth factor-like growth factor (HB-EGF) and epidermal growth factor (EGF), all of which previously had been shown to have altered levels in IC. The average age of participants was 45.7 years. The authors found that APF activity was significantly increased over both normal controls and CP/CPPS patients, while there was no significant difference in CP/CPPS and control groups. Levels of HG-EGF were significantly lower in the IC group as compared to CP/CPPS or control patients, while no significant differences in HG-EGF levels were seen in the latter two. Statistical differences in EGF levels were not seen between any of the three groups. These findings also further differentiate between the pathophysiological mechanisms of IC/BPS and CP/CPPS (22).
Cystoscopy
Historically, a diagnosis of IC in a male was based on a history of bladder pain, irritative voiding symptoms and characteristics findings in the bladder mucosa upon cystoscopy after hydrodistension under anesthesia (23-25). The use of cystoscopy for diagnosis is an essential part of the NIDDK criteria for IC/CPS (20). More recent research has shown such poor sensitivity and specificity of the presence of glomerulations that they have been dropped from the AUA guidelines. Nevertheless, cystoscopy (at least under local anesthesia) can have an important role as part of a hematuria workup, to exclude other pathology, and to look for the presence of Hunner’s ulcers, which, when present, are diagnostic of IC/BPS. At the time of cystoscopy under local anesthetic, lidocaine can be instilled into the bladder as a diagnostic maneuver. Temporary resolution of symptoms may point to the bladder rather than the prostate as the primary pain generator (26).
Clinical phenotyping and UPOINT
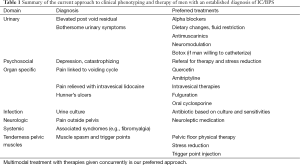
Both CP/CPPS and IC/BPS are heterogeneous conditions that often respond to different therapies. There is a need to phenotype patients in a clinically meaningful way that can guide therapy, much as is done with the TNM classification for cancer. In order to better phenotype patients with CP/CPPS and IC/BPS, the UPOINT system was developed, an acronym for six domains: urinary symptoms, psychosocial dysfunction, organ-specific findings, infection, neurologic/systemic dysfunction, and tenderness of muscles. Rather than managing CP/CPPS from the perspective of characteristic biomarkers or defined pathophysiology, UPOINT takes a phenotypic approach to what is now better understood as a multifactorial problem that often requires multimodal therapy (27). The presence of a greater number of positive domains has been shown to correlate with increasing severity on the Chronic Prostatitis Symptom Index (CPSI) score. The duration of symptoms has also been shown to correlate with the number of positive domains, which supports the hypothesis that ongoing unresolved tissue injury and inflammatory processes further propagate the syndrome and progress to local muscle spasm, central and peripheral neurological changes, and psychosocial changes after the initial insult has cleared (28). Based on the UPOINT phenotype, treatment strategies can be tailored according to the domains in which a patient falls. Previous large multicenter trials have shown limited efficacy for individual available agents as compared to placebo. While the total number of domains may be similar between two patients, the distribution of scores may be vastly different. With this stratification the UPOINT system allows the practitioner to develop a tailored multimodal approach specific for each individual patient based on his pattern of domains. Previous work has shown that multimodal therapy is more effective than monotherapy for CP/CPPS, however prior to the introduction of UPOINT a classification system to guide that therapy had not yet been established (29,30). It should be noted that the UPOINT system was designed to be adaptable to include any new domains to reflect developments in the field such as the discovery of novel biomarkers. Similar to CP/CPPS, trials of single-agent therapy for IC/BPS have struggled from a lack of efficacy, in large part because these multi-faceted disease syndromes are hardly homogenous in their presentation or the universal predominance of a specific symptom. Patients are phenotypically diverse, and so the treatment regimens for each individual patient must be designed based on the phenotype with which a particular patient presents (27). The application of UPOINT to an IC/BPS population has previously been described. At a tertiary referral IC clinic in Ontario, Canada, 100 women were evaluated using the UPOINT classification system. Patients were identified as having “chronic (more than 6 months) pelvic pain, pressure or discomfort perceived to be related to the urinary bladder accompanied by at least one other urinary symptom such as urgency or frequency.” Cystoscopic findings were not part of the inclusion criteria for a diagnosis of IC/BPS. All patients completed the Interstitial Cystitis Symptom Index (ICSI), the pain/urgency/frequency questionnaire, and the visual analogue scale for pain, urgency, and frequency. The authors found that psychosocial dysfunction, infection, neurological, and tenderness of muscles were the most commonly positive domains among study participants. A positive correlation was seen between the number of UPOINT domains a patient experienced and the symptom severity ICSI score as well as the duration of symptoms. The majority of patients were included in the urinary and organ-specific domains, which is not surprising given the explicit inclusion criteria. A fair number of patients were also positive for domains other than organ specific, which the authors note is not surprising given the frequency with which bladder specific treatments often fail. Overall, 72% of patients improved with multimodal therapy driven by the UPOINT phenotype (31).
Treatment
Much like the search for clear mechanisms to explain the etiology of and tests and criteria to develop a definitive diagnosis for IC/BPS, popular treatment options have not been shown to be consistently beneficial. A number of studies have shown improvements in symptom scores in placebo arms as well as treatment arms—often at comparable response levels—without comparable statistical differences between groups (32). Unfortunately long-term outcomes are often disappointing (33). Treatment studies of IC/BPS rarely stratify patients by gender, and patient populations are often heavily skewed towards if not exclusively comprised of women. Very little data is available currently on the treatment of IC/BPS specifically in men, nor acknowledge the gender-specific difficulties inherent in certain treatment options.
Current practice guidelines by the AUA advocate for a stepwise approach to the treatment and management of IC/BPS after other diagnoses are excluded. The guidelines note that “multiple, simultaneous treatments may be considered if it is in the best interests of the patient; baseline symptom assessment and regular symptom level reassessment are essential to document efficacy of single and combined treatments (34).” Furthermore the treatment paradigm does not taken into account gender differences with respect to treatment responses, anatomy, or efficacy. Much of the supporting evidence is based on data from female-only or female-predominant studies, in which gender-stratification of treatment responses is rare. Therapies progress from most to least conservative, with first line treatments centered on patient education and behavioral modification.
Second-line treatments include physical therapy and initiation of oral agents, such as hydroxyzine, amitriptyline, and pentosan polysulfate sodium (PPS), as well as intravesical agents such as lidocaine, heparin, and dimethyl sulfoxide (DMSO). Pelvic floor physical therapy has been shown to be beneficial in CP/CPPS when pelvic floor spasm is present in men, though studies dedicated to determining its utility in men with IC/BPS are unavailable (35). PPS is the only FDA-approved oral medication for the treatment of IC in the United States, despite treatment effects being quite modest (36,37). Recently, Nickel et al. studied the long-term effect of PPS monotherapy versus placebo for the treatment of IC/BPS (38). The study included 36 men and 332 women—which makes it one of the largest single studies of a treatment protocol for IC/BPS to date. Unlike many previous studies, cystoscopy findings consistent with NIDDK criteria were not used for inclusion/exclusion of study participants. Both PPS naïve and PPS non-naïve patients were included. Patients were randomized to PPS 100 mg 3 times daily (the FDA-approved dose), PPS 100 mg daily, or placebo for a period of 24 weeks. Periodic assessment was performed using the ICSI questionnaire, with a >30% reduction in ICSI considered successful treatment response (39). Response rates were 42.6%, 39.8%, and 40.7% respectively, with no statistically significant differences between any of the three groups, indicating that currently-approved therapeutic and subtherapeutic doses of PPS monotherapy were no better than placebo at treating the manifestations of IC/BPS (38). Anecdotally, in our own practice we have been very disappointed by the clinical utility of PPS in men, whether as monotherapy or as part of multimodal therapy and have now abandoned it. For men with the organ specific UPOINT phenotype we prefer such agents as amitriptyline, quercetin (40), and in more advanced cases, cyclosporine (see below).
Third-line therapy consists of cystoscopy with hydrodistension and electrosurgical management of Hunner’s ulcers. What both intravesical and cystoscopic treatments fail to consider is that intravesical and cystoscopic therapies are inherently more challenging in men due to anatomy, and subject men to an increase risk of treatment-related complications down the road including urethral stricture formation from repeated instrumentation as well as the need for increased level of anesthesia. In addition, the effectiveness of intravesical treatments has not been consistent (41). While intravesical lidocaine has been presented as having potential direct therapeutic effects on the suspected neuroinflammatory and mast cell activation components of IC/BPS, studies demonstrating its benefit more commonly employ lidocaine in combination with heparin in intravesical instillations, and even then these studies include very few if any men in their target populations (42-46).
Neuromodulation and intravesical botulinum toxin injections are fourth-line therapies, and cyclosporine, a drug commonly incorporation into transplantation rejection regimens is relegated to fifth-line treatment. Botulinum injections are commonly targeted towards the bladder trigone where the majority of bladder afferent nerve fibers are present (47). Promising results have been shown in a number of studies demonstrating reduction in both pain and irritative voiding complaints (48-53). However study numbers are small, rarely placebo-controlled, and much like investigations assessing lidocaine, contain few if any male participants. Furthermore the use of intravesical botulinum toxin carries a much higher risk of urinary retention in men, a complicating factor that must be taken into account when appropriately counseling a male patient.
The use of cyclosporine for the treatment of IC/BPS was borne from the theory that IC/BPS has a significant autoimmune component, and was sometimes found in association with Sjogren’s syndrome (54,55). Since its first application to IC/BPS in the 1990’s, a number of studies have shown therapeutic long-term benefit in its use in both men and women (56,57). Better results have been seen in patients who present with Hunner’s ulcers than those without, and with greater clinical effect on both symptom questionnaires and voiding symptoms when compared to patients treated with PPS monotherapy (56,58,59). We have had surprisingly good success with cyclosporine therapy in men, whether or not Hunner’s ulcers are present. We typically start at 3 mg/kg in two divided doses (much lower than the doses used in organ transplantation) and reduce the dose to 2 mg/kg if possible once clinical efficacy is seen. Patients need regular monitoring of blood pressure and renal function while on therapy, and while we have seen side effects including hypertension and increased serum creatinine, so far all have been temporary and have resolved or improved with dose reduction or cessation. The mechanism of action and most appropriate use in IC/BPS is currently being studied under a National Institutes of Health funded protocol with results expected in 2016.
Sixth and final line treatments include urinary diversion with or without cystectomy and substitution cystoplasty, which have shown good results in some studies which have included both men and women, but given the drastic nature of the intervention this is only reserved as a last resort when other therapies have failed (60,61).
In the predecessor to their 2004 study, Forrest and colleagues present one of the few case series of treatment outcomes specifically in men with IC/BPS. A total of 52 patients treated for IC from 1990-2000 at a single clinic were included. Exclusions were made for any history of positive bacterial localization cultures. All diagnoses were made using the NIDDK Consensus Conference criteria. Treatments were based largely on availability at the time of therapy initiation. Seven of the 52 patients were treated with intravesical DMSO with good initial response but treatment failure within 6 months. Thirty-seven patients were treated with a multi-drug regimen of pentosan sodium sulfate, amitriptyline, and an anticholinergic agent. At the 3-month mark, 80% of these patients reported a 75% improvement in their symptoms, with a durable treatment response at 1 year from treatment initiation. Only two of the 37 patients reported no improvement at all, while two patients endorsed complete resolution. Eight of the 52 patients were treated with amitriptyline and an anticholinergic agent, and 75% were considered to have failed therapy (11). The authors did not report the degree of success of the remaining two patients. This study is one of the few that specifically studies treatment outcomes in men with IC/BPS, demonstrating durable treatment responses with multi-drug regimens.
Conclusions
While all men with CP/CPPS do not have IC/BPS, there are many men who do have IC/BPS and can benefit from IC/BPS specific therapies such as fulguration of ulcers, intravesical therapy and cyclosporine. The heterogeneity of patient presentations has made it difficult to clearly classify and treat these patients effectively and in a timely manner, particularly in men, as it is relatively recent that the presence and scope of IC/BPS in men is being acknowledged. Better screening options are needed to diagnose comorbid conditions, pain disorder, sexual dysfunction and psychosocial issues in men. Current treatment guidelines are limited by a lack of thorough, well-planned clinical trials in the literature, and available treatment options have met with mixed results, and have rarely been validated specifically in the treatment of men with IC/BPS.
The development of UPOINT has led to successful multimodal therapy based on the spectrum of patient-specific phenotypes in CP/CPPS, and has been successfully validated and applied to the treatment of IC/BPS in women. Further research is needed to determine the efficacy of available treatment options in afflicted males, and treatment guidelines need to be updated from a step-wise approach to a simultaneous, multimodal approach in order to effectively treat IC/BPS in men. Our current approach to phenotyping and treating men with IC/BPS is summarized in Table 1.
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: DA Shoskes is a consultant to Farr Laboratories, Tribute Pharmaceuticals, Astellas Pharma, and Eli Lilly. HC Arora has no conflicts of interest to declare.
References
- Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2011;185:2162-70. [PubMed]
- Teichman JM, Parsons CL. Contemporary clinical presentation of interstitial cystitis. Urology 2007;69:41-7. [PubMed]
- Oravisto KJ. Epidemiology of interstitial cystitis. Ann Chir Gynaecol Fenn 1975;64:75-7. [PubMed]
- Clemens JQ, Meenan RT, Rosetti MC, et al. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol 2005;173:98-102; discussion 102. [PubMed]
- Forrest JB, Nickel JC, Moldwin RM. Chronic prostatitis/chronic pelvic pain syndrome and male interstitial cystitis: enigmas and opportunities. Urology 2007;69:60-3. [PubMed]
- Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology 2001;57:428-32; discussion 432-3. [PubMed]
- Novicki DE, Larson TR, Swanson SK. Interstitial cystitis in men. Urology 1998;52:621-4. [PubMed]
- Forrest JB, Schmidt S. Interstitial cystitis, chronic nonbacterial prostatitis and chronic pelvic pain syndrome in men: a common and frequently identical clinical entity. J Urol 2004;172:2561-2. [PubMed]
- Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA 1999;282:236-7. [PubMed]
- Nickel JC, Alexander RB, Anderson R, et al. Category III chronic prostatitis/chronic pelvic pain syndrome: insights from the National Institutes of Health Chronic Prostatitis Collaborative Research Network studies. Curr Urol Rep 2008;9:320-7. [PubMed]
- Forrest JB, Vo Q. Observations on the presentation, diagnosis, and treatment of interstitial cystitis in men. Urology 2001;57:26-9. [PubMed]
- Berger RE, Miller JE, Rothman I, et al. Bladder petechiae after cystoscopy and hydrodistension in men diagnosed with prostate pain. J Urol 1998;159:83-5. [PubMed]
- Berry SH, Elliott MN, Suttorp M, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol 2011;186:540-4. [PubMed]
- Hall SA, Link CL, Pulliam SJ, et al. The relationship of common medical conditions and medication use with symptoms of painful bladder syndrome: results from the Boston area community health survey. J Urol 2008;180:593-8. [PubMed]
- Suskind AM, Berry SH, Ewing BA, et al. The prevalence and overlap of interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome in men: results of the RAND Interstitial Cystitis Epidemiology male study. J Urol 2013;189:141-5. [PubMed]
- Miller JL, Rothman I, Bavendam TG, et al. Prostatodynia and interstitial cystitis: one and the same? Urology 1995;45:587-90. [PubMed]
- Hanno PM. Bladder pain syndrome (interstitial cystitis) and related disorders. In: Wein AJ, Kavoussi LR, Novick AC, et al, editors. Campbell-Walsh Urology. Philadelphia: Elsevier Saunders, 2012:357-401.
- Koziol JA. Epidemiology of interstitial cystitis. Urol Clin North Am 1994;21:7-20. [PubMed]
- Hanno PM. Interstitial cystitis-epidemiology, diagnostic criteria, clinical markers. Rev Urol 2002;4 Suppl 1:S3-8. [PubMed]
- Gillenwater JY, Wein AJ. Summary of the National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases Workshop on Interstitial Cystitis, National Institutes of Health, Bethesda, Maryland, August 28-29, 1987. J Urol 1988;140:203-6. [PubMed]
- Hanno PM, Landis JR, Matthews-Cook Y, et al. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol 1999;161:553-7. [PubMed]
- Keay S, Zhang CO, Chai T, et al. Antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor in men with interstitial cystitis versus chronic pelvic pain syndrome. Urology 2004;63:22-6. [PubMed]
- Evans RJ, Sant GR. Current diagnosis of interstitial cystitis: an evolving paradigm. Urology 2007;69:64-72. [PubMed]
- Nickel JC. Textbook of Prostatitis. CRC Press; 1999:378.
- Sant GR. Etiology, pathogenesis, and diagnosis of interstitial cystitis. Rev Urol 2002;4 Suppl 1:S9-S15. [PubMed]
- Henry RA, Morales A, Cahill CM. Beyond a Simple Anesthetic Effect: Lidocaine in the Diagnosis and Treatment of Interstitial Cystitis/bladder Pain Syndrome. Urology 2015;85:1025-33. [PubMed]
- Shoskes DA, Nickel JC, Rackley RR, et al. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis 2009;12:177-83. [PubMed]
- Pontari MA, Ruggieri MR. Mechanisms in prostatitis/chronic pelvic pain syndrome. J Urol 2008;179:S61-7. [PubMed]
- Nickel JC, Downey J, Ardern D, et al. Failure of a monotherapy strategy for difficult chronic prostatitis/chronic pelvic pain syndrome. J Urol 2004;172:551-4. [PubMed]
- Cohen JM, Fagin AP, Hariton E, et al. Therapeutic intervention for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): a systematic review and meta-analysis. PLoS One 2012;7:e41941. [PubMed]
- Nickel JC, Shoskes D, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome: a key to classification and potentially improved management. J Urol 2009;182:155-60. [PubMed]
- Bosch PC. Examination of the significant placebo effect in the treatment of interstitial cystitis/bladder pain syndrome. Urology 2014;84:321-6. [PubMed]
- Propert KJ, Schaeffer AJ, Brensinger CM, et al. A prospective study of interstitial cystitis: results of longitudinal followup of the interstitial cystitis data base cohort. The Interstitial Cystitis Data Base Study Group. J Urol 2000;163:1434-9. [PubMed]
- Hanno PM, Erickson D, Moldwin R, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol 2015;193:1545-53. [PubMed]
- Polackwich AS, Li J, Shoskes DA. Patients with Pelvic Floor Muscle Spasm Have a Superior Response to Pelvic Floor Physical Therapy at Specialized Centers. J Urol 2015;194:1002-6. [PubMed]
- Janssen Pharmaceuticals. Elmiron®-100 MG (pentosan polysulfate sodium) capsules prescribing information description. Cited Aug 9, 2015. Available online: http://www.orthoelmiron.com/sites/default/files/assets/elmiron.pdf
- Parsons CL, Benson G, Childs SJ, et al. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. J Urol 1993;150:845-8. [PubMed]
- Nickel JC, Herschorn S, Whitmore KE, et al. Pentosan polysulfate sodium for treatment of interstitial cystitis/bladder pain syndrome: insights from a randomized, double-blind, placebo controlled study. J Urol 2015;193:857-62. [PubMed]
- O’Leary MP, Sant GR, Fowler FJ Jr, et al. The interstitial cystitis symptom index and problem index. Urology 1997;49:58-63. [PubMed]
- Katske F, Shoskes DA, Sender M, et al. Treatment of interstitial cystitis with a quercetin supplement. Tech Urol 2001;7:44-6. [PubMed]
- Dawson TE, Jamison J. Intravesical treatments for painful bladder syndrome/ interstitial cystitis. Cochrane Database Syst Rev 2007.CD006113. [PubMed]
- Lv YS, Zhou HL, Mao HP, et al. Intravesical hyaluronic acid and alkalinized lidocaine for the treatment of severe painful bladder syndrome/interstitial cystitis. Int Urogynecol J 2012;23:1715-20. [PubMed]
- Nomiya A, Naruse T, Niimi A, et al. On- and post-treatment symptom relief by repeated instillations of heparin and alkalized lidocaine in interstitial cystitis. Int J Urol 2013;20:1118-22. [PubMed]
- Parsons CL. Successful downregulation of bladder sensory nerves with combination of heparin and alkalinized lidocaine in patients with interstitial cystitis. Urology 2005;65:45-8. [PubMed]
- Parsons CL, Koziol JA, Proctor JG, et al. Heparin and alkalinized lidocaine versus alkalinized lidocaine for treatment of interstitial cystitis symptoms. Can J Urol 2015;22:7739-44. [PubMed]
- Parsons CL, Zupkas P, Proctor J, et al. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. J Sex Med 2012;9:207-12. [PubMed]
- Pinto R, Lopes T, Frias B, et al. Trigonal injection of botulinum toxin A in patients with refractory bladder pain syndrome/interstitial cystitis. Eur Urol 2010;58:360-5. [PubMed]
- Kuo HC. Repeated intravesical onabotulinumtoxinA injections are effective in treatment of refractory interstitial cystitis/bladder pain syndrome. Int J Clin Pract 2013;67:427-34. [PubMed]
- Jhang JF, Jiang YH, Kuo HC. Potential therapeutic effect of intravesical botulinum toxin type A on bladder pain syndrome/interstitial cystitis. Int J Urol 2014;21 Suppl 1:49-55. [PubMed]
- Akiyama Y, Nomiya A, Niimi A, et al. Botulinum toxin type A injection for refractory interstitial cystitis: A randomized comparative study and predictors of treatment response. Int J Urol 2015;22:835-41. [PubMed]
- Tirumuru S, Al-Kurdi D, Latthe P. Intravesical botulinum toxin A injections in the treatment of painful bladder syndrome/interstitial cystitis: a systematic review. Int Urogynecol J 2010;21:1285-300. [PubMed]
- Ramsay AK, Small DR, Conn IG. Intravesical botulinum toxin type A in chronic interstitial cystitis: results of a pilot study. Surgeon 2007;5:331-3. [PubMed]
- Kuo HC, Jiang YH, Tsai YC, et al. Intravesical botulinum toxin-A injections reduce bladder pain of interstitial cystitis/bladder pain syndrome refractory to conventional treatment - A prospective, multicenter, randomized, double-blind, placebo-controlled clinical trial. Neurourol Urodyn 2015. [Epub ahead of print]. [PubMed]
- Emmungil H, Kalfa M, Zihni FY, et al. Interstitial cystitis: a rare manifestation of primary Sjögren’s syndrome, successfully treated with low dose cyclosporine. Rheumatol Int 2012;32:1215-8. [PubMed]
- Forsell T, Ruutu M, Isoniemi H, et al. Cyclosporine in severe interstitial cystitis. J Urol 1996;155:1591-3. [PubMed]
- Sairanen J, Forsell T, Ruutu M. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. J Urol 2004;171:2138-41. [PubMed]
- Sairanen J, Hotakainen K, Tammela TL, et al. Urinary epidermal growth factor and interleukin-6 levels in patients with painful bladder syndrome/interstitial cystitis treated with cyclosporine or pentosan polysulfate sodium. Urology 2008;71:630-3. [PubMed]
- Forrest JB, Payne CK, Erickson DR. Cyclosporine A for refractory interstitial cystitis/bladder pain syndrome: experience of 3 tertiary centers. J Urol 2012;188:1186-91. [PubMed]
- Sairanen J, Tammela TL, Leppilahti M, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol 2005;174:2235-8. [PubMed]
- Kim HJ, Lee JS, Cho WJ, et al. Efficacy and safety of augmentation ileocystoplasty combined with supratrigonal cystectomy for the treatment of refractory bladder pain syndrome/interstitial cystitis with Hunner’s lesion. Int J Urol 2014;21 Suppl 1:69-73. [PubMed]
- Rössberger J, Fall M, Jonsson O, et al. Long-term results of reconstructive surgery in patients with bladder pain syndrome/interstitial cystitis: subtyping is imperative. Urology 2007;70:638-42. [PubMed]


