Does normalizing PSA after successful treatment of chronic prostatitis with high PSA value exclude prostatic biopsy?
Introduction
The prostate-specific antigen (PSA) level has considered an essential diagnostic method for detecting prostate cancer. The abnormal digital rectal examination (DRE) has been obviously reduced and biochemical result (elevated PSA) have augment the indication of prostate biopsy over the past 20 years (1). Men with high PSA of more than 4 ng/mL are considered to be at higher risk for prostate cancer and should be recommended to perform prostate biopsy (2).
Nevertheless, increased PSA is not essentially associated with prostate cancer, but can also elevate in conditions away from cancerous lesions, such as prostate inflammation, bacterial prostatitis, benign prostatic hyperplasia (BPH) and urinary tract infection (3-5).
The recommended cutoff value of PSA for needle biopsy to detect cancer prostate has lately been decreased to 2.5 ng/mL (2). As many investigators had documented the potential incidence of prostate cancer in men with a PSA <4 ng/mL (4).
Many studies have investigated the relationship of serum PSA and prostate inflammation to give the clue of the debate whether prostate biopsies could be excluded by treatment of chronic prostatitis and lowering of PSA (5,6). The majority of these studies founded that detection and treatment of prostatitis may decrease PSA and consequently decrease the number of patients provided for prostate biopsy for cancer diagnosis. On the other hand, the most important weakness of the reported studies is that pathologic examinations are not obtainable for patients with a post-treatment PSA level <4 ng/mL because they did not perform a prostate biopsy.
In our study, we evaluated men with diagnosed chronic prostatitis and elevated serum PSA to find out if the treatment with antibiotics and anti-inflammatory drugs can decrease PSA level or not.
Besides, we proceeded to prostate biopsy for all patients after treatment and examine the cancer detection rate in patients with variable PSA values.
Patients and methods
This prospective study was performed for 142 male patients aged 40-73 years, who came to the outpatient clinic between January 2009 and May 2011 with symptoms &signs suggesting chronic prostatitis [lower urinary tract symptoms (LUTS); dysuria; perineal, or pelvic pain; painful ejaculation] with PSA >4 ng/mL. Excluded patients who had bladder disease (tumors, stones and neurogenic bladder), urethral stricture, urine retention, urethral catheter insertion, previous history of prostatic surgery or biopsy. Also patients with abnormal findings during digital rectal examination (DRE) of prostate which include (palpable nodules, prostatic indurations, hardness, asymmetry and prostatic fluctuation) and patients with previous intake of 5-alpha reductase inhibitors were excluded. All patients underwent detailed medical history and clinical examination (general & local). Chronic prostatitis was confirmed if expressed prostatic secretion (EPS) obtained from digital prostatic massage reveled more than 10 white blood cells per high power field.
Patients fulfilling these findings received a full course of medical treatment consisting of fluoroquinolone antibiotic (ofloxacin 400 mg/day) and non-steroid anti inflammatory (piroxicam 20 mg/day) for 6-weeks duration. Subsequently, all patients were followed-up by PSA and transrectal ultrasound- guide needle biopsy (TRUS) within 2 months after treatment. The PSA level was determined by using immunoenzymatic assay. TRUS procedure was performed using a 7.5 MHz probe and at least 10 core prostatic biopsy specimens obtained by biopsy gun and an 18-guage needle biopsy. Prophylactic antibiotics were given to all patients (ofloxacin 400 mg/day, 5 days) starting the day prior the biopsy. All prostatic specimens were pathologically examined. Patients enrolled in this study were given informed consent for their contributions and TRUS.
Results
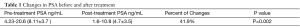
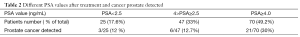
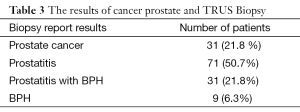
The enrolled patients were 142 men with chronic prostatitis and elevated PSA >4 ng/mL, their mean age was (54.4±13.5) years, the mean PSA pretreatment was (8.11±3.7) ng/mL. After 6 weeks of combined treatment with an antibiotic and non-steroid anti-inflammatory drugs, the mean PSA denoted a significant decrease to (4.7±3.5) ng/mL (P=0.002). The recorded percent of changes in mean PSA before and after treatment was 41.9% (Table 1). The observed post-treatment PSA values were, PSA<2.5 in 25 patients, 4.0>PSA≥2.5 in 47 patients and PSA≥4.0 in 70 patients (Table 2). The observed results of TRUS and biopsy after treatment were, cancer prostate found in 31 patients (21.8%), chronic prostatitis in 71 patients (50.7%), chronic prostatitis plus benign prostatic hyperplasia (BPH) in 31 (21.8%) and BPH in 9 patients (6.3%) (Table 3). We observed decrease in PSA below 4 ng/mL in 72 patients (50.7%) of the total 142 patients with high PSA >4 ng/mL after treatment. With regard to PSA values, the documented cancer prostate patients were 3/25 (12%) if PSA <2.5 ng/mL, 6/47 (12.7%) if 4.0>PSA≥2.5 and 21/70 (30%) if PSA≥4.0. The estimated numbers of cancer prostate detected patients were 30 (21.1%) (Table 2). Technical statistics were performed by use of SPSS ver. 10.0 (SPSS Inc., Chicago, IL, USA), and independent t-tests were used for analysis. P-values of less than 0.05 were considered significant.
Full table
Full table
Full table
Discussion
The diagnostic rate of prostate cancer has been escalating since PSA was used in the evaluation in the 1980s as a method for detecting prostate cancer (7). Although, the abnormal finding on a DRE or TRUS used as an indication for prostate biopsy, but the high PSA level confirm the decision of prostate biopsy (8). However, some prostatic diseases can give high PSA values due to the specificity and sensitivity of PSA (9). The PSA could increase in BPH, urinary tract infection, urinary obstruction, bacterial prostatitis and prostatic interventions such as prostate massage, prostate biopsy and transurethral resections (10). The PSA might elevated in acute inflammation and silent infection. In addition, some investigators have reported that treatment of chronic prostatitis with antibiotics and anti-inflammatory drugs decline the PSA value and the need for prostate biopsy (11).
Pansadoro et al. (12) found that PSA elevated in 71% of patients with acute prostatitis, 15% of patients with chronic prostatitis, and 6% of patients with nonbacterial prostatitis. In addition, Hasui et al. (13) documented increase in the PSA with acute and chronic prostatitis supported by clinical symptoms and confirmed histological.
Many investigators had documented that treatment of chronic prostatitis could decline the PSA level, which clear that the use of antimicrobial or nonsteroidal anti-inflammatory drugs may diminish the need of prostate biopsy (14,15). These reports have raised the difficulty of how to direct men with elevated PSA and chronic prostatitis.
In the current study, we reported that the mean PSA was significantly decreased after 6 weeks of treatment with antibiotics and nonsteroidal anti-inflammatory drugs, the percentage of change in PSA before and after treatment was 41.9%. We reported that, PSA in 72 of 142 (50.7%) of the patients with elevated PSA declined to the normal range (PSA<4 ng/mL) after 6 weeks of treatment. Between those patients, the PSA value was less than 2.5 ng/mL in 25 patients (17.6%). In addition, the prostate cancer diagnosed rate after treatment was, 12%, 12.7%, and 30%, if PSA<2.5, 4.0>PSA≥2.5 and PSA≥4.0 ng/mL respectively.
A retrospective study performed by Bozeman et al. (16), analyzed that, ninety-five patients with an elevated PSA and inflammation in expressed prostatic secretions who underwent medications with antibiotics and anti-inflammatory drugs for 4 weeks. They declare that, the PSA value decreased by 36% from the baseline after medications with antibiotics and nonsteroidal anti-inflammatory drugs in patients with chronic prostatitis and that 44 (46.3%) of the patients had post-treatment PSA values of <4 ng/mL, therefore avoiding biopsy, whereas the lasting 51 (53.7%) proceeded to biopsy, detected the presence of cancer in 13 (25.5%). They finally founded that their positive biopsy rate enhanced from 13.7% to 25.5% with preliminary treatment of chronic prostatitis.
The main controversy of that study described above and our report are that, the biopsy was performed only in patients with post-treatment PSA levels still elevated >4 ng/mL but not performed in all patients. Decrease the PSA level may not eliminate the need of a prostate biopsy to exclude the existence of prostate cancer
According to the potential incidence of prostate cancer with a PSA level lower than 4 ng/mL, the advised cutoff value of PSA for prostatic needle biopsy was lately decreased to 2.5 ng/mL (17). Gilbert et al. (18) reported that, prostate cancer detection rate in patients with a PSA level of 2.5 to 4 ng/mL (27.48%) and patients with a PSA level between 4 and 10 ng/mL (30.8%).
Also, Thompson et al. (19) reported that, 14% of men with a PSA level between 2.5 and 4 ng/mL had biopsy-detectable prostate cancer and that findings are comparable to our findings.
Stopiglia et al. (20), conducted the prospective study of the PSA changes after treatment with antibiotics in patients with prostatitis and elevated PSA. They included patients with a PSA<2.5 ng/mL in the prostate biopsy procedure and unexpectedly found a quite high rate of cancer (30%) in those with a PSA even lower than 2.5 ng/mL during the follow-up. They conclusively stated that, in patients with normalized levels of PSA (below 2.5 ng/mL), the absence of prostate cancer is not confirmed, and must be not respected in the decision to perform prostate biopsy or not.
Our report are supported also by Baltaci et al. (21), whose reported that while antibiotic therapy will reduce total serum PSA, it will not drop off the risk of prostate cancer, even if the PSA level decline to less than 4 g/mL.
Conclusions
The results of the current study make obvious that chronic prostatitis is one of the causes that can lead to elevation of serum PSA levels. Treatment of chronic prostatitis with elevated PSA by antibiotics and anti-inflammatory agents can decrease the elevated PSA to the normal levels. Nevertheless, the opportunity of clinically potential prostate cancer remains in patients with a decreased PSA level of less than 4 ng/mL, even also if PSA decreases to less than 2.5 ng/mL. Consequently, the need for needle biopsy to detect prostate cancer can not be excluded in those patients with normal values of PSA after treatment of chronic prostatitis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Roberts RO, Bergstralh EJ, Lieber MM, et al. Digital rectal examination and prostate-specific antigen abnormalities at the time of prostate biopsy and biopsy outcomes, 1980 to 1997. Urology 2000;56:817-22. [PubMed]
- Catalona WJ, Ramos CG, Carvalhal GF, et al. Lowering PSA cutoffs to enhance detection of curable prostate cancer. Urology 2000;55:791-5. [PubMed]
- Dalton DL. Elevated serum prostate-specific antigen due to acute bacterial prostatitis. Urology 1989;33:465. [PubMed]
- Cho IR, Kim GJ, Park SS, et al. PSA and Prostatitis in Men under 45 Years Old. Korean J Urol 1998;39:633-7.
- Ozden C, Ozdal OL, Guzel O, et al. The correlation between serum prostate specific antigen levels and asymptomatic inflammatory prostatitis. Int Urol Nephrol 2007;39:859-63. [PubMed]
- Erol H, Beder N, Calişkan T, et al. Can the effect of antibiotherapy and anti-inflammatory therapy on serum PSA levels discriminate between benign and malign prostatic pathologies? Urol Int 2006;76:20-6. [PubMed]
- Lee DH, Yang WJ, Chung BH, et al. A Multicenter Study of the Detection Rate for Prostate Cancer according to the Serum Prostate-Specific Antigen Level in Korean Men. Korean J Urol 2005;46:433-7.
- Nelson WG, De Marzo AM, Isaacs WB. Prostate cancer. N Engl J Med 2003;349:366-81. [PubMed]
- Carver BS, Bozeman CB, Williams BJ, et al. The prevalence of men with National Institutes of Health category IV prostatitis and association with serum prostate specific antigen. J Urol 2003;169:589-91. [PubMed]
- Morote J, Lopez M, Encabo G, et al. Effect of inflammation and benign prostatic enlargement on total and percent free serum prostatic specific antigen. Eur Urol 2000;37:537-40. [PubMed]
- Bulbul MA, Wazzan W, Hijaz A, et al. The effect of antibiotics on elevated serum prostate specific antigen in patients with urinary symptoms and negative digital rectal examination: a pilot study. J Med Liban 2002;50:23-5. [PubMed]
- Pansadoro V, Emiliozzi P, Defidio L, et al. Prostate-specific antigen and prostatitis in men under fifty. Eur Urol 1996;30:24-7. [PubMed]
- Hasui Y, Marutsuka K, Asada Y, et al. Relationship between serum prostate specific antigen and histological prostatitis in patients with benign prostatic hyperplasia. Prostate 1994;25:91-6. [PubMed]
- Potts JM. Prospective identification of National Institutes of Health category IV prostatitis in men with elevated prostate specific antigen. J Urol 2000;164:1550-3. [PubMed]
- Stancik I, Lüftenegger W, Klimpfinger M, et al. Effect of NIH-IV prostatitis on free and free-to-total PSA. Eur Urol 2004;46:760-4. [PubMed]
- Bozeman CB, Carver BS, Eastham JA, et al. Treatment of chronic prostatitis lowers serum prostate specific antigen. J Urol 2002;167:1723-6. [PubMed]
- Nadler RB, Humphrey PA, Smith DS, et al. Effect of inflammation and benign prostatic hyperplasia on elevated serum prostate specific antigen levels. J Urol 1995;154:407-13. [PubMed]
- Gilbert SM, Cavallo CB, Kahane H, et al. Evidence suggesting PSA cutpoint of 2.5 ng/mL for prompting prostate biopsy: review of 36,316 biopsies. Urology 2005;65:549-53. [PubMed]
- Thompson IM, Pauler DK, Goodman PJ, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med 2004;350:2239-46. [PubMed]
- Stopiglia RM, Ferreira U, Silva MM Jr, et al. Prostate specific antigen decrease and prostate cancer diagnosis: antibiotic versus placebo prospective randomized clinical trial. J Urol 2010;183:940-4. [PubMed]
- Baltaci S, Süer E, Haliloğlu AH, et al. Effectiveness of antibiotics given to asymptomatic men for an increased prostate specific antigen. J Urol 2009;181:128-32. [PubMed]


