Commentary on refractory ischemic priapism
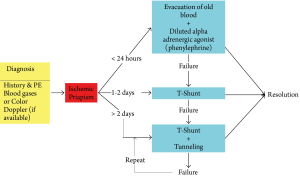
In our experience treating more than 100 cases of ischemic priapism, we noted that most with less than 24-hour duration responded well to aspiration/evacuation and injection of a diluted alpha-adrenergic agent (phenylephrine). In those of less than 48-hour duration, the majority could be reversed by a standard T-shunt with #10 blade. In those who failed T-shunt or had more than 48-hour duration, T-shunt with tunneling was effective for the vast majority of patients. However, there are always exceptions to any general rule. The following two educational cases represent an example where a repeat T-shunt with tunneling procedure was needed to reverse the priapism. The various comments below illustrate sub-optimal management by less experienced urologists and our recommendations for the same situations. This report will also introduce a new "Duration-directed Algorithm" (Figure 1), which we believe represents a more physiologic approach. In addition, we also propose a method to estimate ischemia time for standardize reporting of treatment outcome in clinical series.
Case presentation I
A 36 year-old man was referred to our urology service for management of ischemic priapism refractory to multiple medical and surgical treatments. The patient reported awakening one morning with a rigid erection, which, as the day progressed, became painful.
1st procedure: Forty-eight hours after onset, he presented to a local hospital complaining of severe penile pain, where he was managed initially with needle aspiration, injection of diluted phenylephrine (Comment 1), and application of an ice-pack. These treatments failed.
2nd procedure: Later on the same day, he underwent glans-cavernosum shunts with a needle. This too failed.
3rd procedure: The following morning (Day 3), he underwent bilateral glans-cavernosum T-shunt, using an 11-blade scalpel (Comment 2), which resulted in several hours of relief, but the painful, rigid erection returned.
4th procedure: The following morning (Day 4), the patient underwent a Left spongiosum-cavernosum shunt, at the peno-scrotal junction (Comment 3). The rigid, painful erect state soon returned. On the evening of Day 5 the patient was transferred to our institution for further management.
The patient reported only two prior episodes of prolonged erections, both within the preceding two weeks. The first lasted 8 hours and spontaneously resolved, and the second lasted 10 hours and resolved only after needle aspiration.
He denied any history of use of erectogenic medications, drugs, or penile trauma. He denied any personal or family history of sickle–cell disease. The patient described his erectile function and penile sensation as normal and satisfactory for intercourse.
On initial exam, he was noted to have a rigid, painful erection. He was uncircumcised, and had phimosis due to significant foreskin swelling. The distal 2/3 of his penile skin was ecchymotic. A small eschar was present on the skin at the left-distal aspect of his penile shaft. A 16 Fr. Foley catheter was in place and draining faintly blood-tinged urine without clots. The patient was afebrile. Laboratory analyses were notable for a WBC of 11×103/mm3 and urine analysis showed 11-20 RBC and <5 WBC per high power field.
5th procedure: After discussion of management options and the risks and benefits, the patient was taken to the operating room, where he underwent bilateral T-shunt with a #10 blade scalpel, bilateral intracavernosal tunneling with a 22-Fr. straight urethral sound, which was advanced to the base of the penis. Dark ischemic blood was manually expressed from the penis until bright-red blood was visible. Circumcision was performed to prevent paraphimosis. At completion of surgery, the penis was partially erect but could be compressed easily. Given the presence of micro-hematuria and concern for an occult urethral injury, a new urethral catheter was inserted, and left this in place for 7 days (Comment 4).
Hospital course: Shortly after surgery, the patient reported significant reduction of the intense, constant, dull penile pain he experienced before surgery. He received intravenous (IV) Zosyn for 24-hour peri-operatively, and then was switched to an oral antibiotic (Cephalexin). His post-op urine analysis continued to show micro-hematuria. Urine culture remained negative. The morning after surgery, he was ambulating without assistance, tolerating a regular diet, and had adequate pain control with oral analgesics. He was discharged home on post-operative day #1 with prescriptions for 7 days of Cephalexin 500 mg QID (antibiotic), and Pentoxifylline 400 mg orally every 8 hours with meals ×6 months.
Follow-up: The patient reported complete resolution of the deep, dull penile pain which is characteristic of ischemic priapism pain within 36 hours after surgery. Discomfort at the sutured glans incision-sites resolved completely within 5 days after surgery. On exam, the incision sites were healing well, and ecchymosis was nearly entirely resolved. A cystourethroscopy was performed, and revealed a 4 mm × 3 mm. urethral injury at the 5 O'Clock position on the left, inferior-lateral aspect of the penile urethra, 5.5 cm from the urethral meatus. The patient was contacted by phone about 4 months after surgery. He reported return of nocturnal erections approximately 3 weeks after surgery, and return of normal erections (without the need for phosphodiesterase inhibitors) 6-weeks after surgery. At follow-up, his SHIM score was 25 (Comment 5).
Case presentation II
27 year-old otherwise healthy male with prior history of a 4-hour spontaneously resolving priapism approximately 4 months ago presented to ED with priapism for 36 hours. Patient denied inciting factors including drugs and medications.
1st procedure: Patient was seen at a community hospital where aspiration and injection of phenylephrine were attempted without success; he was subsequently sent to the emergency department of our hospital for further management.
2nd procedure: On admission, the patient was able to void without hematuria or dysuria. At that time 800 mL of blood was aspirated from the corpora at bedside (Comment 6), but the penis remained erect. Phenylephrine 500 mcg was injected into the corpora bilaterally at 3 min intervals, with a total of 20 mg. There was no evidence of detumescence following these procedures.
3rd procedure: Under local anesthesia, a bedside T-shunt was performed using an #11 blade scalpel (Comment 2), which was inserted dorsolaterally to the meatus on both sides, and rotated (blade-edge) 90-degrees laterally. This resulted in rapid detumescence. Therefore, the tunneling procedure was not performed. Approximately 200 mL of moderately dark blood was evacuated from glans wound sites. These were closed with interrupted 3-0 chromic sutures (Comment 7). The patient was started on oral Ciprofloxacin (twice daily) and pentoxyphylline (three times per day). UA and UCx were negative for blood or infection, respectively, and WBC was within normal range and remained stable after admission.
4th procedure: On hospital day #2, ischemic priapism returned and a color duplex penile ultrasound revealed no blood flow in the cavernous arteries. The patient was taken to the operating room for repeat T-shunt and bilateral tunneling. The sutures were removed and a #10 blade was used. Tunneling was performed with a 22F straight female sound, resulting in rapid detumescence. The patient reported pain relief after the procedure, however, his erection returned to 75% rigidity 8-10 hours after procedure. The antibiotic was changed to oral Keflex, 500 mg every 6 hours. On hospital day #3 the penis remained unchanged. Ketoconazole was started to reduce nocturnal erections and the urethral catheter was removed.
On hospital day #4, the penis was 100% erect. The patient continued to use on-demand IV analgesia, and oral ibuprofen, Percocet, Dilaudid, and oxycodone for additional pain control. However, he denied complete pain relief. At this time he was still able to urinate without a urethral catheter.
5th Procedure: On hospital day #6, there was no reduction in tumescence and edema. Bedside T-shunt with tunneling was again performed using a #10 blade scalpel. Intravenous Dilaudid, Ativan, and bupivicaine penile block were administered for pain relief and sedation. The previous shunts were clotted. Dark blood was expressed from the opened shunts. The patient tolerated the repeat procedure well. Aspirin (325 mg) and Pepcid (40 mg) daily were commenced. (Comment 8). He developed urinary retention that required insertion of a Foley urethral catheter.
Hospital day #7: The penis remained edematous and partially tumescent, but the patient reported decreased pain. On Hospital day #8 the penis was 90% detumesced, and edema had significantly improved. The urethral catheter was removed. The patient was discharged on Hospital day #10 with a prescription for aspirin (81 mg) and Pepcid (40 mg), each daily, for 2 weeks, Keflex antibiotic for 5 additional days, Ketoconazole for 2 more days (to reduce night-time erections), and Pentoxyfylline (to reduce intracorporal scarring) for 6 months. During the hospital course, the patient's hematocrit dropped from 36.2 to 26.1, but he remained asymptomatic. He returned to our clinic for follow-up evaluation 4 weeks later, and a color duplex ultrasound revealed excellent flow in both corpora cavernosa. He reported that nocturnal erections began to return 3 weeks after discharge from hospital. He reported normal penile sensation and denied pain with erections.
On follow-up evaluation at 6 weeks, the patient reported that erections of 70% rigidity (compared to baseline erectile function) returned 6 weeks after discharge home. These erections were described as sufficient for penetration, but of shorter duration as compared to baseline function. The patient had not yet tried oral PDE-5 inhibitors.
Expert opinions
Description of T-shunt and corporal tunneling surgical procedures
As described previously (1), the tips of the firm corporal bodies are palpated through the (normally) soft glans 1-2 mL of 0.25% Bupivicaine is injected subcutaneously (just blow the skin) on the glans. A circumferential block at the base of the penis is optional. A 10-blade scalpel is positioned vertically, inserted into the corpus cavernosum and advanced until the hub of the blade is at skin level. The sharp-edge of the blade is then rotated 90-degree laterally, and withdrawn.
Dark ischemic blood is expressed manually until the return is fresh and bright-red. The glans wound is closed and the patient is observed for 15 minutes. If rigid erection returns, the same procedure is performed on the other side. If the dark ischemic blood drained out slowly, and the penis remained partially erect after expression of old blood (this usually occurs when priapism has lasted for >2-3 days), and severe edema of the intracavernous tissue is evident, bilateral tunneling via the same incisions should be performed. This is achieved with a 20- to 22-Fr. straight urethral sound. The surgeon should first estimate the length of the sound that will be inserted in order for the tip of the sound to reach the base of the penile shaft. The sound is held parallel to the long axis of the penis. It is inserted slowly and angled slightly laterally, so as to minimize risk of urethral injury. The base of the penis shaft is then grasped firmly, and dark (ischemic) blood is manually expressed from the incision site(s) until replaced by bright-red blood.
Incision site closure and Assessment
A 4-0 chromic suture is used to close the incision with running, locking sutures. Care taken to avoid placing the sutures too deeply, as deep closure can close the shunt. After closure, the penis is observed, to assess for resolution of the rigid state.
After 15 minutes, rigidity can be assessed by using the thumb and index fingers to squeeze the corporal bodies at mid-shaft. (For priapism events lasting greater than ~48 hours, it is normal for the penis shaft to be firm from local edema, even after the corporal bodies have been drained of trapped ischemic blood.) The shunt is considered open if the (awake) patient reports relief of constant dull ache within the penis (as is present in the rigid ischemic state), and if the penis is sufficiently soft that a 1-1.5 cm indentation can be made by the surgeon's fingers. If the penis returns to a rigid (priapism) state even after wound closure, we recommend repeating the tunneling once (bilaterally).
Wound dressing
The glans suture sites are dressed with antibiotic ointment for 5 days. The shaft should never be dressed with a restrictive dressing (e.g., Coband or other elastic bandages), as these may compress the dorsal vein and the corpus spongiosum, and thus close the shunts).
Comment 1: Although needle aspiration/drainage of ischemic blood, followed by injection/irrigation with diluted alpha adrenergic agent is generally successful for ischemic priapism of less than 24 hours duration, this approach is virtually "useless" for priapism of >48 hours duration, because of tissue edema, absence of intracorporal circulation, and the inability of cavernous smooth muscles to respond to medication. Our preferred approach is a T-shunt or T-shunt with tunneling.
Comment 2: Immediately after the ischemic state is corrected, a large amount of arterial flow rushes into the corpora cavernosa. This is due to "post-ischemic hyperemia" and it may last for hours to days. Without a large shunt to receive the excessive volume of inflow, the intracavernous pressure will soon rise and compress the tissue surrounding the outlet, effectively closing the shunt. The shunt created by a #11 blade is small and can easily close spontaneously. We prefer the larger incision offered by a #10 blade, and we rotate the blade 90-degrees laterally as it is withdrawn to make a "T-shaped" shunt, which ultimately serves to maximize the size of the shunt.
Comment 3: The purpose of a cavernosum-spongiosum shunt is to drain blood from the corpora cavernosa to the urethral bulb in the perineum. Anatomically, the spongy tissue that surrounds the male penile urethra is relatively thin. However, at the level of the bulbar urethra, the thickness of spongiosal tissue is several times greater. If a shunt is created at the level of the peno-scrotal junction, the thin layer of spongiosal tissue present is inadequate to drain the corporal body. Furthermore, the thin nature of the spongiosal tissue at this level increases the risk of urethral injury. The authors have seen several cases of cavernositis followed by caverno-urethral-cutaneous fistula and complete occlusion of the urethra, followed by subsequent severe cavernosal fibrosis, when a shunt is placed too distally. Given the simple technique and efficacy of the cavernosum-glans shunt with tunneling procedure we describe (1-4), we do not see a need for proximal shunting procedures.
Comment 4: The presence of hematuria and a history of recent spongiosum-cavernosum shunt should raise a red flag about urethral injury. To prevent the complications mentioned in Comment #3, it is important to place a urethral catheter and administer antibiotics for several days.
Comment 5: Currently, there is no standard definition of the "duration" of an ischemic priapism, and this may account for why it is difficult to interpret the efficacy and treatment outcomes reported in the literature. Theoretically, if no treatment is given after 5 days of ischemic priapism, the penile erectile tissue should be completely necrotic and any shunting procedure would fail to restore potency. In this case, although our T-shunt with tunneling procedure (which reversed the priapism state) was performed 5 days after onset, the patient had already undergone multiple procedures (on days 3 and 4) to evacuate old blood and re-establish circulation, each of which resulted in temporary detumescence. During the brief period of detumescence, the ischemic state is interrupted, hypoxia is reversed, and tissues receive oxygenated blood flow. Blood flow helps to eliminate accumulated metabolic wastes. Therefore, in this patient, the longest continuous ischemia time was really only approximately 48 hours. We believe that both the patient's young age and the only 48-hour period of continuous ischemia can account for the return of erectile function we observed.
Comment 6: The purpose of aspiration/evacuation is to remove old, ischemic/acidotic blood and to facilitate return of fresh, oxygenated blood. Usually aspiration of 100-150 mL. is sufficient to achieve this. In our view, there is no need to drain more than 200 mL. of blood during aspiration.
Comment 7: Because of the rich blood supply of the glans, interrupted suture may not be able to achieve hemostasis. We recommend use of a running-locking suture.
Comment 8: Physiologically, the shunt will not close if the shunt is large enough to accommodate the reactive high arterial flow after the ischemia is reversed. This post-ischemic hyperemia, or "reactive high-flow state", usually lasts hours to days. A T-shunt created by a (smaller) #11 blade may not be adequate to drain high-volume arterial flow. The resulting build-up of high pressure is the likely cause of premature shunt closure in the two cases described above. The failure to maintain an open shunt after a #10 blade T-shunt in the second case may be due to severe local tissue edema, which can impede drainage across the shunt. For this reason, we gave the patient both aspirin (to prevent shunt clotting) and ketoconazole (to reduce nocturnal erections). Alternatively, a standard Al-Ghorab shunt (surgical excision of the tip of both corpora cavernosa) with tunneling can be performed (4). We prefer repeated T-shunt and tunneling because this can be performed at bedside, using only local anesthesia. Use of repeat #10-blade T- shunt with tunneling has been successful in reversing refractory priapism for all cases where initial use of T-shunt and tunneling failed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Garcia MM, Shindel AW, Lue TF. T-shunt with or without tunnelling for prolonged ischaemic priapism. BJU Int 2008;102:1754-64. [PubMed]
- Brant WO, Garcia MM, Bella AJ, et al. T-shaped shunt and intracavernous tunneling for prolonged ischemic priapism. J Urol 2009;181:1699-705. [PubMed]
- Burnett AL, Pierorazio PM. Corporal "snake" maneuver: corporoglanular shunt surgical modification for ischemic priapism. J Sex Med 2009;6:1171-6. [PubMed]
- Lian W, Lv J, Cui W, et al. Al-Ghorab Shunt plus intracavernous tunneling for prolonged ischemic priapism. J Androl 2010;31:466-71. [PubMed]